Introduction
Shingles, also known as herpes zoster, is a viral infection that affects millions of people worldwide each year. It is caused by the reactivation of the varicella-zoster virus, the same virus responsible for chickenpox. After recovering from chickenpox, the virus remains dormant in the nerve tissues, and in certain conditions, it can reactivate later in life as shingles.
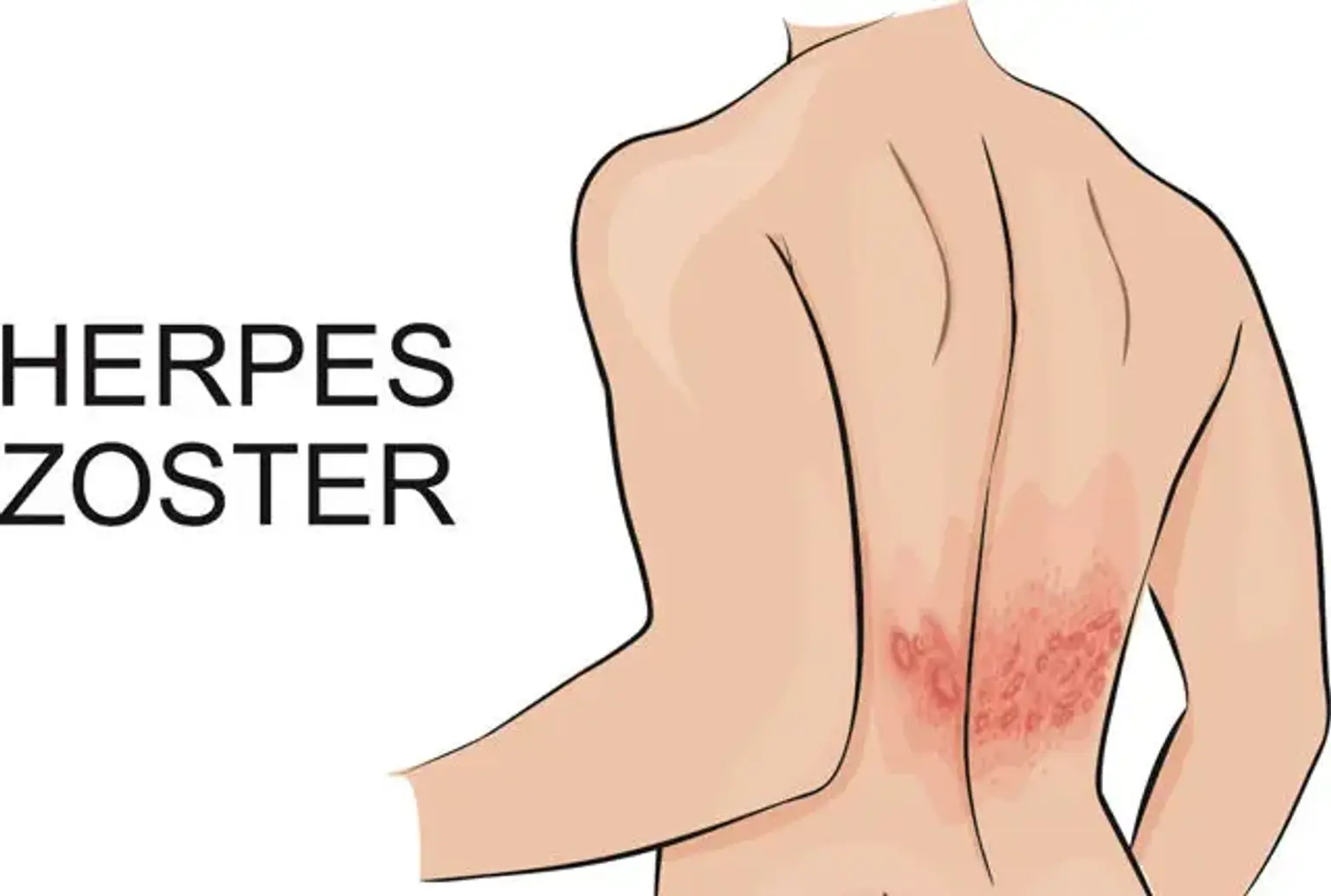
Characterized by a painful rash and blisters, shingles can significantly impact the quality of life, especially in older adults and those with weakened immune systems. The good news is that shingles is both treatable and preventable. Understanding its symptoms, causes, and treatment options is essential to managing this condition effectively.
What Causes Shingles?
The root cause of shingles lies in the reactivation of the chickenpox virus or varicella-zoster virus, which can remain latent in the body for decades. Factors that contribute to the reactivation include:
Aging: The immune system naturally weakens with age, increasing the risk of shingles in people over 50.
Weakened Immunity: Conditions such as HIV/AIDS, cancer, or the use of immunosuppressive drugs can trigger shingles.
Stress: High levels of stress may also compromise immunity and contribute to the virus's reactivation.
Shingles is more prevalent in elderly individuals, making vaccination and proactive health measures critical in this population.