Overview
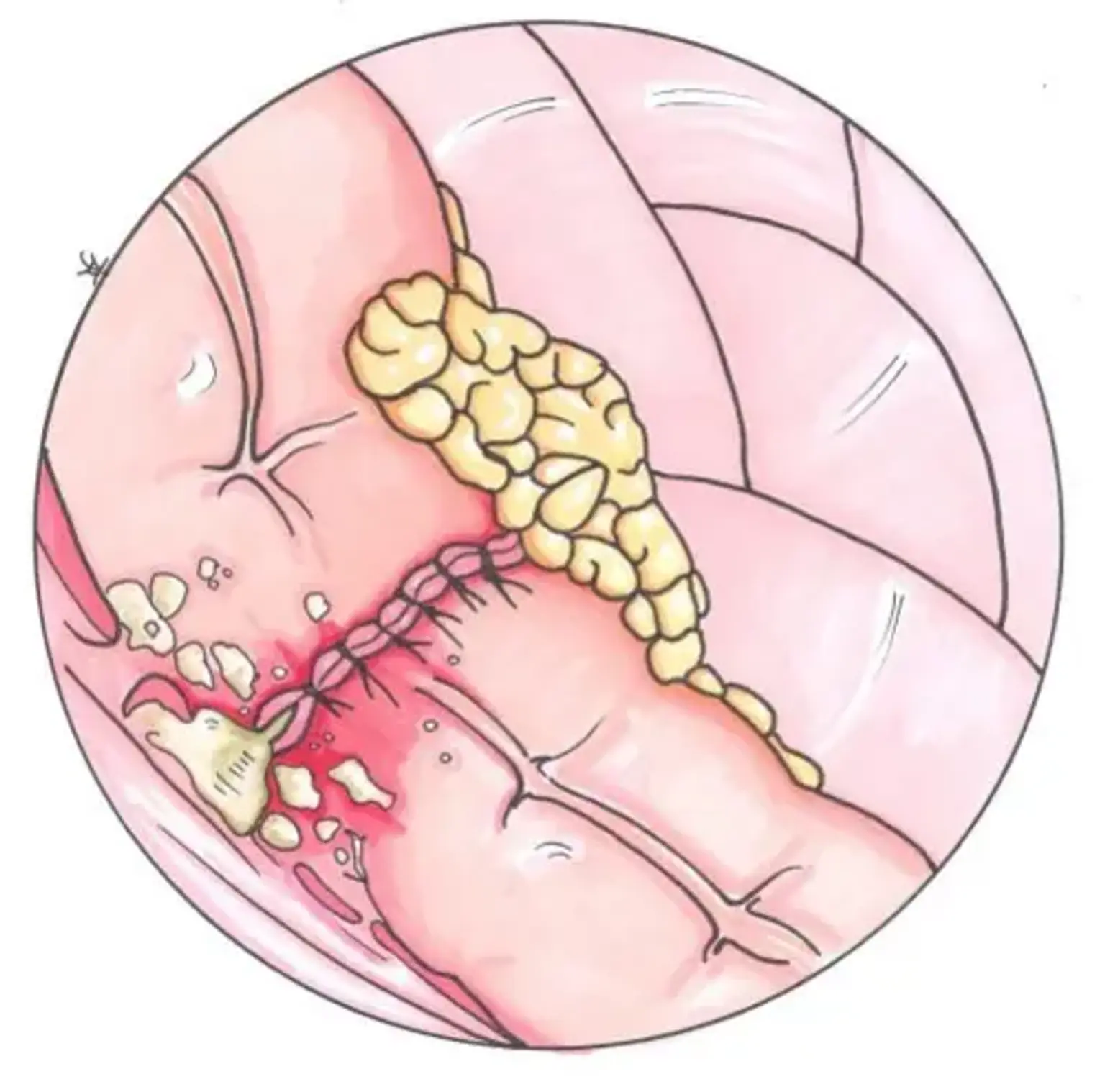
An anastomotic leak occurs when there is a break or hole in the anastomosis, allowing the contents of the bowel or other organs to leak out. This can cause infection, inflammation, and can be life-threatening if not treated in time. Symptoms of an anastomotic leak can include fever, abdominal pain, and a high white blood cell count. Treatment may include antibiotics, drainage of the leak, and in severe cases, surgery to repair or remove the damaged portion of the anastomosis.