Introduction
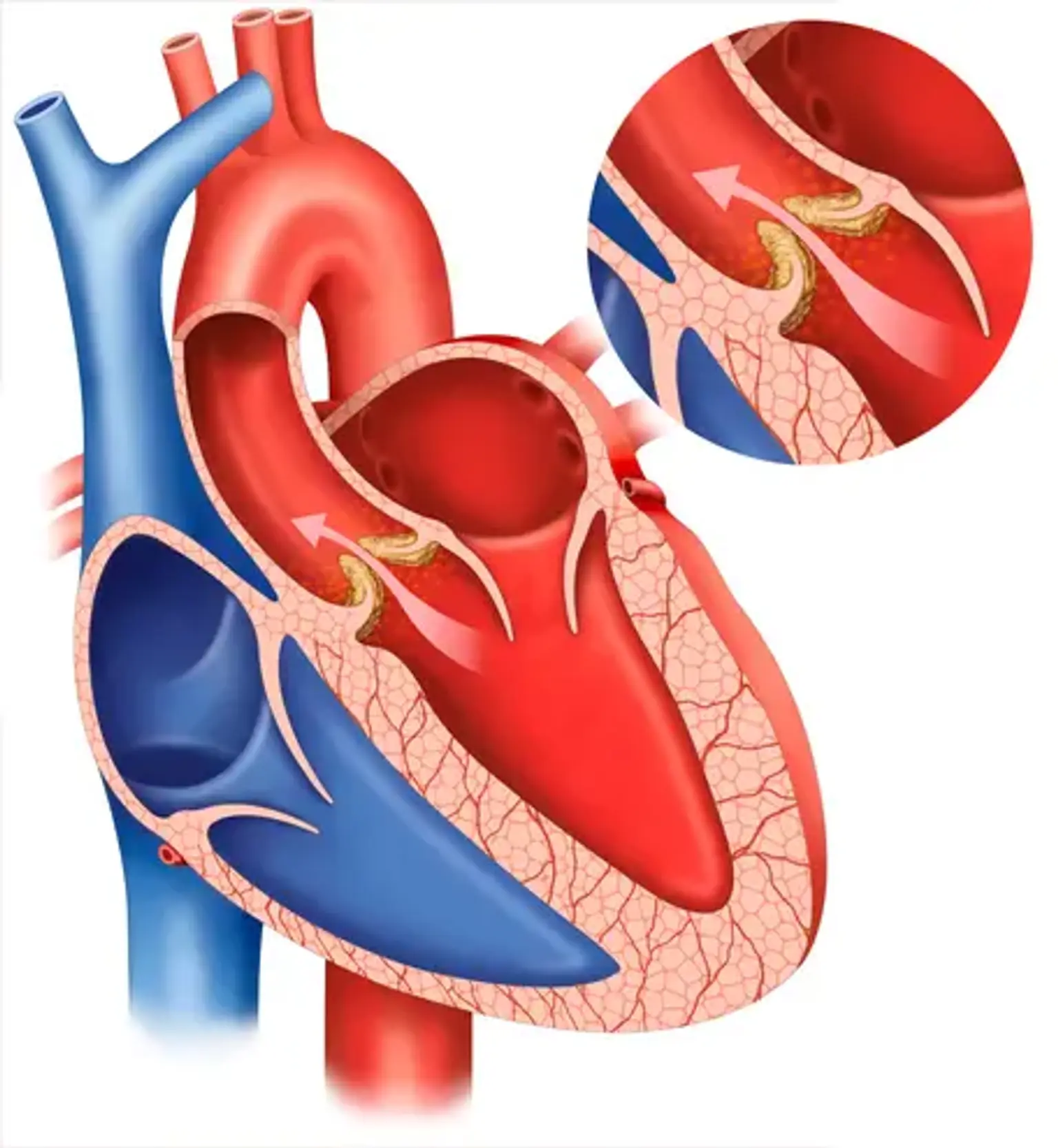
Aortic regurgitation (AR) is a condition characterized by the inability of the aortic valve to close properly, causing blood to flow backward into the left ventricle instead of forward into the aorta. This regurgitation disrupts the heart's efficiency, forcing it to work harder to pump blood, which over time can weaken the heart muscle. If left untreated, AR may lead to severe complications such as left ventricular hypertrophy, arrhythmias, or even congestive heart failure. While the condition can develop gradually over years, some cases progress rapidly, requiring immediate medical attention.
The management of aortic regurgitation begins with a comprehensive understanding of its symptoms, diagnosis, and treatment options. Early detection plays a critical role in mitigating risks and improving outcomes. Recent advancements in diagnostic techniques and surgical interventions have significantly enhanced the prognosis for patients with AR.
In the realm of cardiovascular healthcare, South Korea has become a global frontrunner, renowned for its cutting-edge medical technologies, skilled practitioners, and patient-centered care. Many international patients are drawn to Korea's healthcare system, which combines advanced diagnostics with innovative treatment strategies at competitive costs. This article offers an in-depth exploration of aortic regurgitation, focusing on its symptoms, diagnostic methods, and treatment options while highlighting why Korea is a leading destination for cardiac care.
Symptoms of Aortic Regurgitation
Early Symptoms of Aortic Regurgitation
The symptoms of aortic regurgitation often depend on the severity and rate of progression of the condition. In the early stages, AR may remain asymptomatic or exhibit subtle signs that are easily overlooked. Patients might experience fatigue and reduced exercise tolerance, often attributing these to aging or general lack of fitness. Shortness of breath during physical activity, lightheadedness, and palpitations are other early symptoms that may signal the onset of AR.
One of the hallmark findings in early AR is a heart murmur, often detected during routine check-ups. A heart murmur is an abnormal sound heard during a heartbeat, typically caused by turbulent blood flow due to the leaky aortic valve. While not all murmurs are indicative of severe conditions, their presence warrants further investigation, especially in individuals at risk of heart valve disorders.