Many people worry sometimes about the white stuff that grows in their mouths. They grab a tongue scrubber and try to remove these whitish patches but it doesn’t help.
They are insecure because their mouths look funny and feel weird like sandpaper.
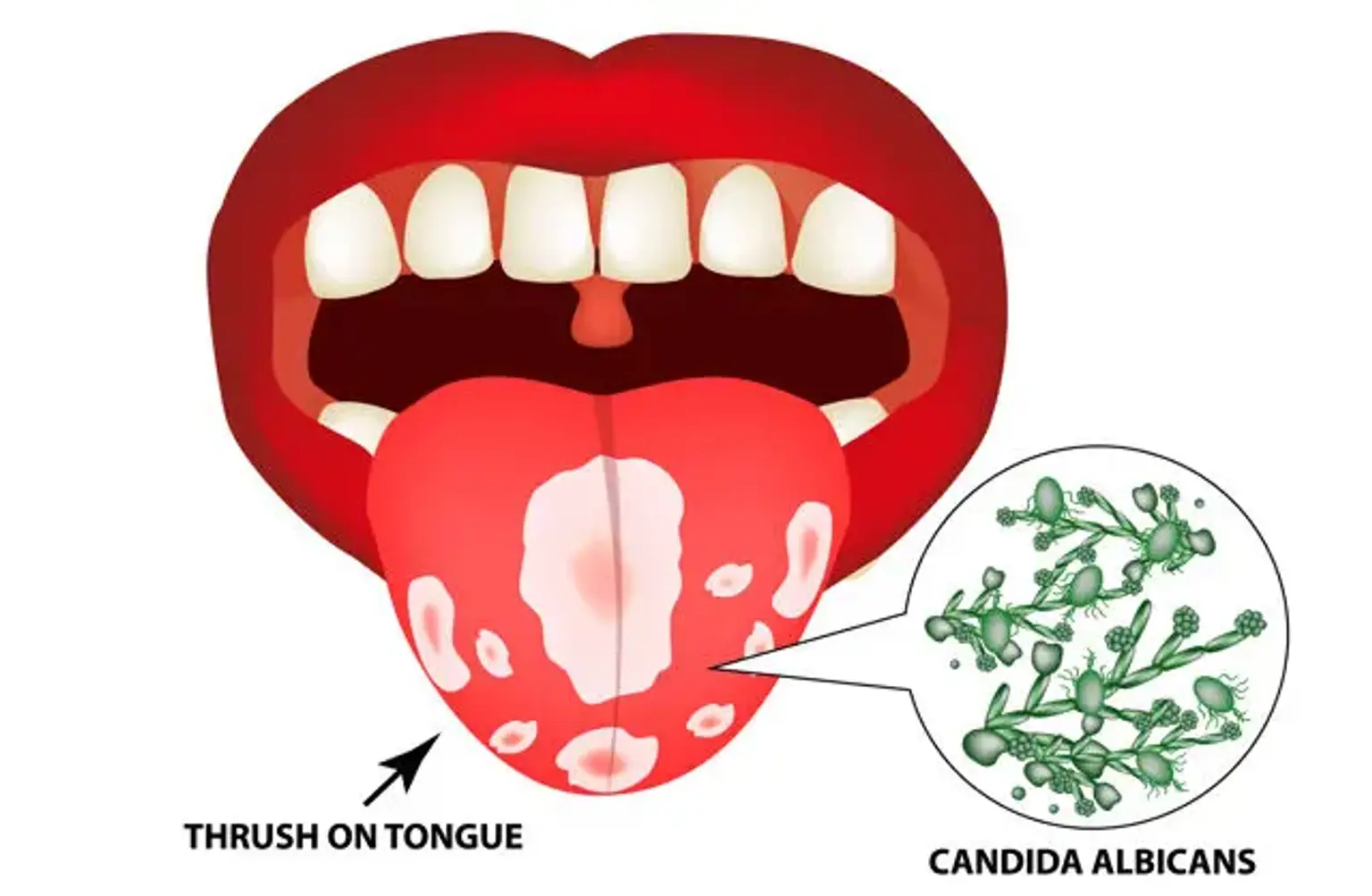
Well, my friend, these people might have thrush.
The mouth, this oval-shaped cavity that contains many structures inside of it, is just like any other organ. It can get different infections and diseases.