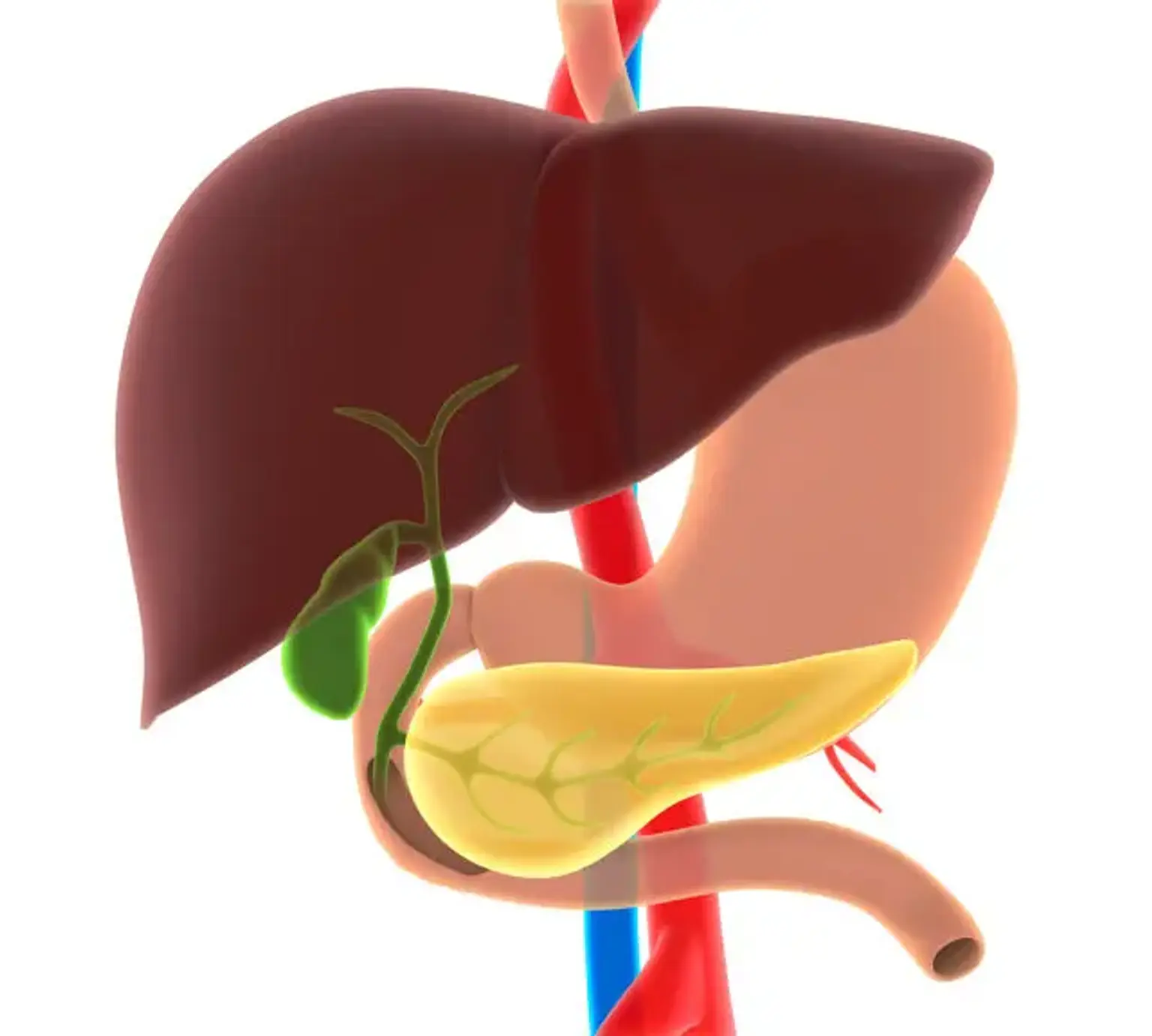
The liver, gallbladder, bile duct, and pancreas are essential in ensuring our day-to-day survival. It helps facilitate bodily functions and ensures that we remain healthy and active at all times. However, these organs are also susceptible to a wide range of health conditions. If you suspect any related disorders, you should immediately seek medical attention to prevent more damages.
Good digestion requires a functioning pancreas and biliary tract. Because pancreatic and biliary tract problems can cause severe conditions that need a fast, precise diagnosis and treatment.
Hepatobiliary and pancreatic surgery is an effective treatment option for complex diseases of the pancreas, liver, gallbladder, and bile duct. It’s mainly recommended if other treatment options, including medication and other non-surgical options, fail to address the issue.