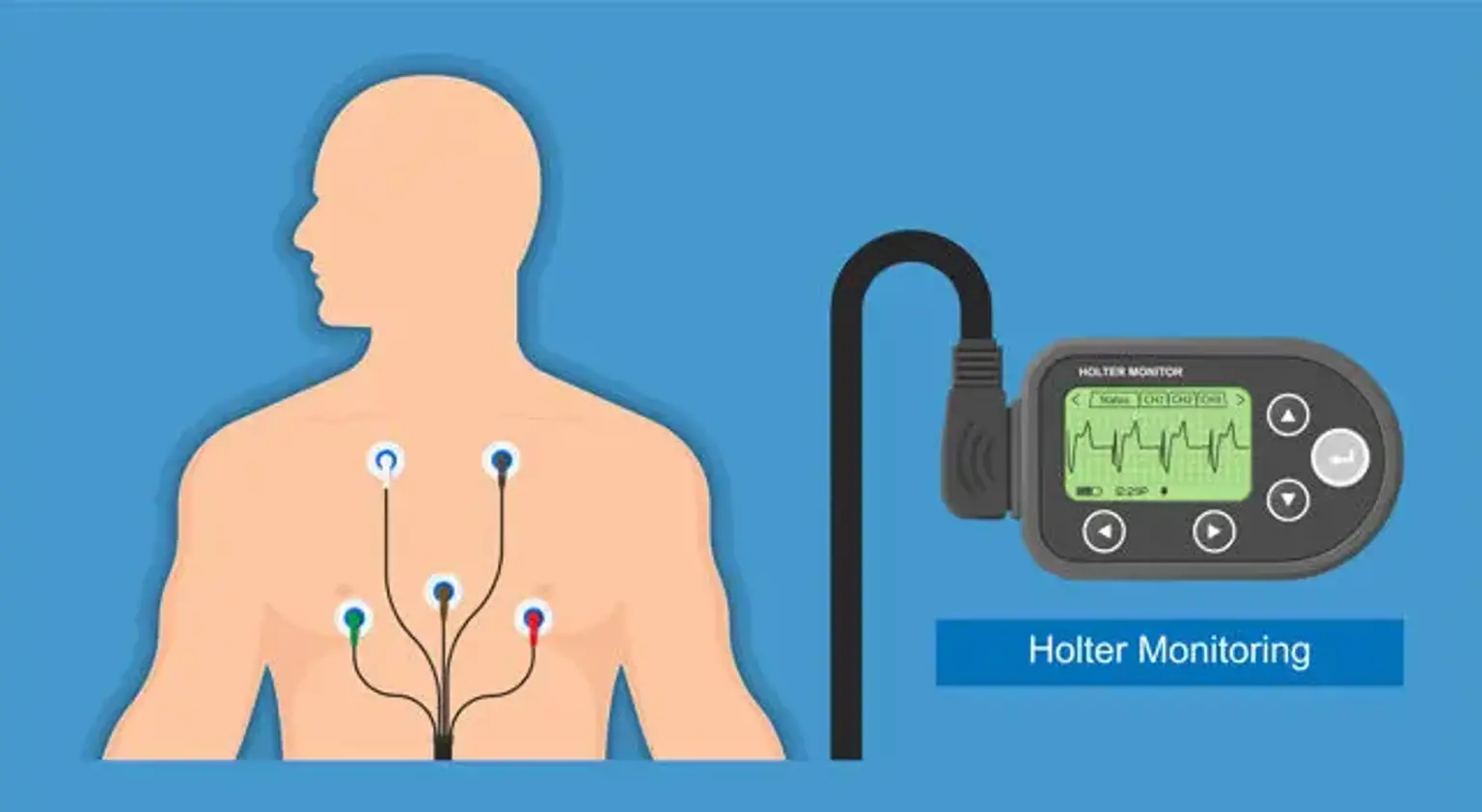
24hr Holter Monitoring
Palpitation is among the most prevalent problems noticed by primary care doctors and cardiologists when they consult outpatients. Although it is normally harmless, it can occasionally be a sign of life-threatening diseases. Because historical clues are not always reliable, determining the source of palpitations can be challenging. The majority of patients with arrhythmias do not experience palpitations. Palpitations are often caused by any type of arrhythmia, including sinus tachycardia, atrial fibrillation, premature ventricular contractions, or ventricular tachycardia.
The Holter analysis is recommended by the American College of Cardiology and the American Heart Association for individuals who have unexplainable fainting, near syncope, palpitations, or dizziness as class I indications for symptomatic assessment. If the causative disease of the palpitations cannot be diagnosed from the patient's history, physical assessment, and ECG, Holter monitoring is usually recommended, but the yield of this instrument is low in individuals whose symptoms occur occasionally.