Anterior cruciate ligament reconstruction (ACL reconstruction)
Overview
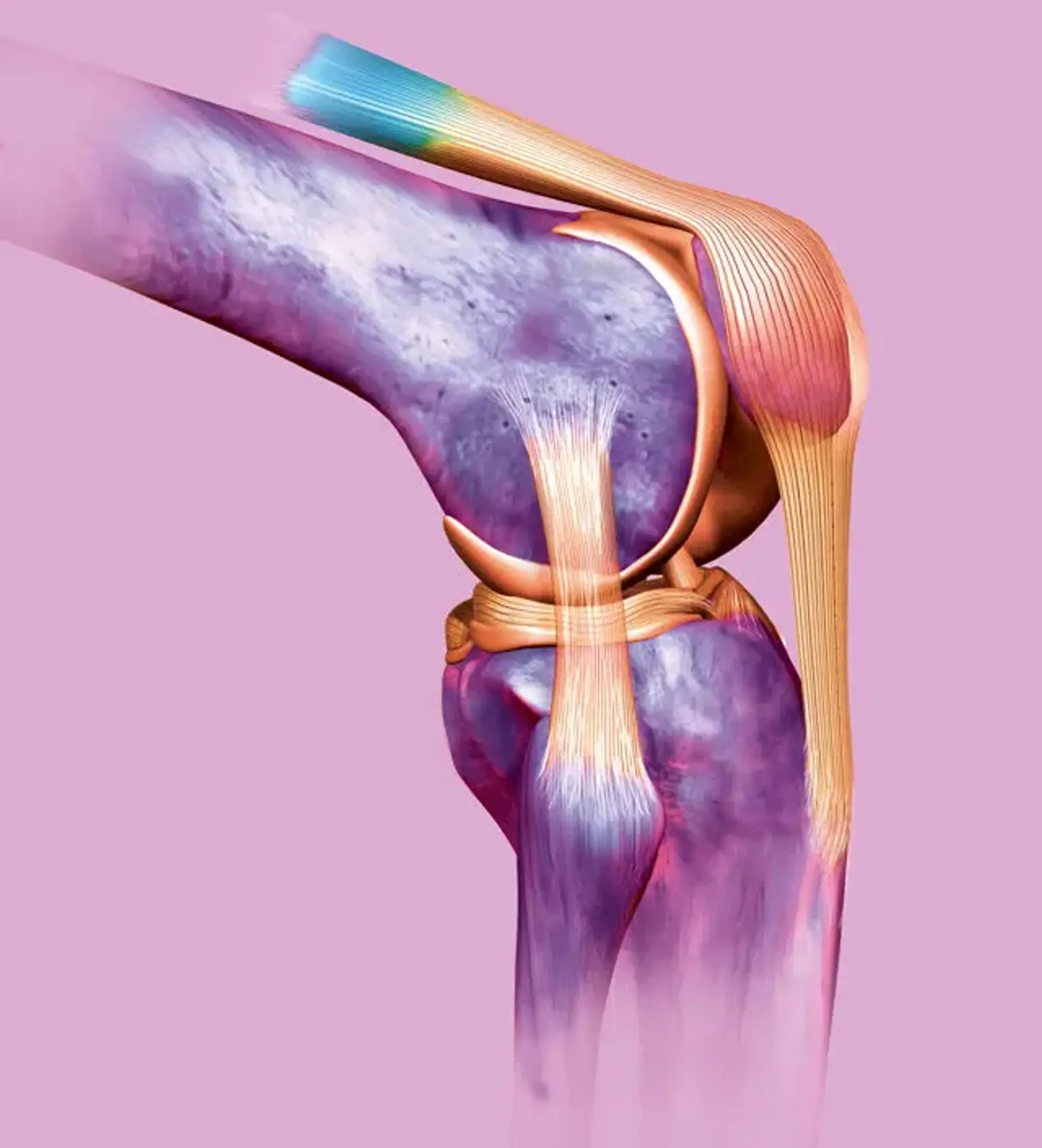
One of the two cruciate ligaments that help to stabilize the knee joint is the anterior cruciate ligament. It is a strong band of connective tissue and collagenous fibers that extends posteromedially from the anteromedial aspect of the tibial plateau's intercondylar region to the lateral femoral condyle. It is the most commonly injured ligament in the knee, and it is most commonly seen in football, soccer, and basketball players.
The ACL and the PCL form a cross (or a "x") within the knee, preventing excessive forward or backward motion of the tibia relative to the femur during flexion and extension. The ACL also provides rotational stability to the knee when it is stressed in Varus or valgus. ACL sprains and tears are common knee injuries, with 100,000 to 200,000 cases reported each year in the United States.