Arterial Switch
Overview
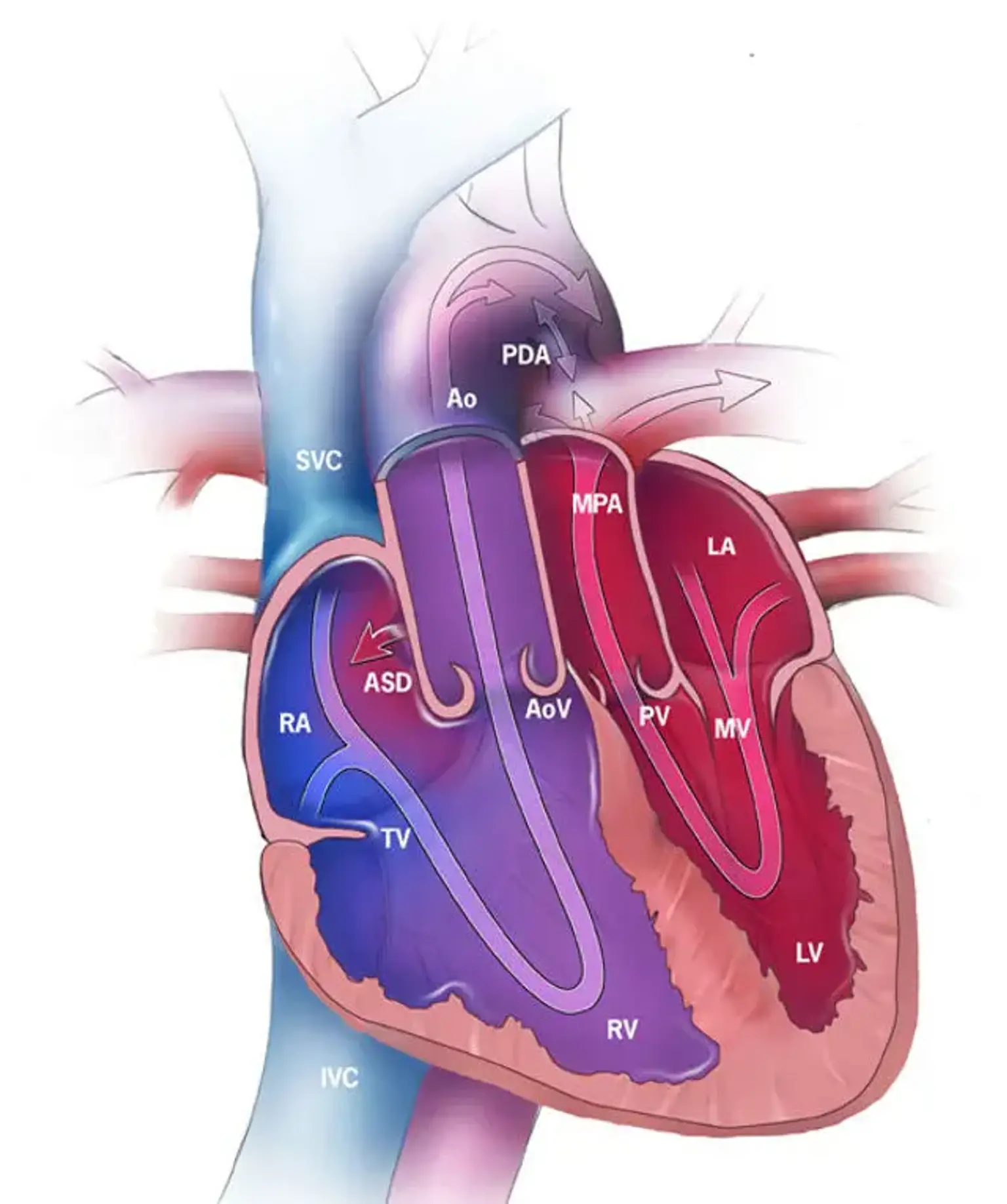
Arterial switch is a surgical procedure and the primary treatment for great artery transposition (TGA). The two major arteries leaving the heart are connected to the wrong ventricles, the two lower chambers of the heart, in transposition of the great arteries. As a result, oxygen-rich blood from the lungs is pumped back into the lungs, while oxygen-depleted blood, which is required to nourish the body, is pumped throughout the body.
Almost all TGA children have their arterial switches repaired. Babies with TGA become very ill soon after birth due to a severe lack of oxygen.
The arterial switch procedure is the primary treatment for correcting transposition of the great arteries (TGA). An arterial switch procedure is an open heart surgery that re-establishes normal blood flow in your baby's body. The aorta is detached from the right atrium and connected to the left atrium during surgery; the pulmonary artery is detached from the left atrium and tied to the right atrium; and the coronary arteries are cut out of the pulmonary artery and attached to the aorta.