Arthroplasty
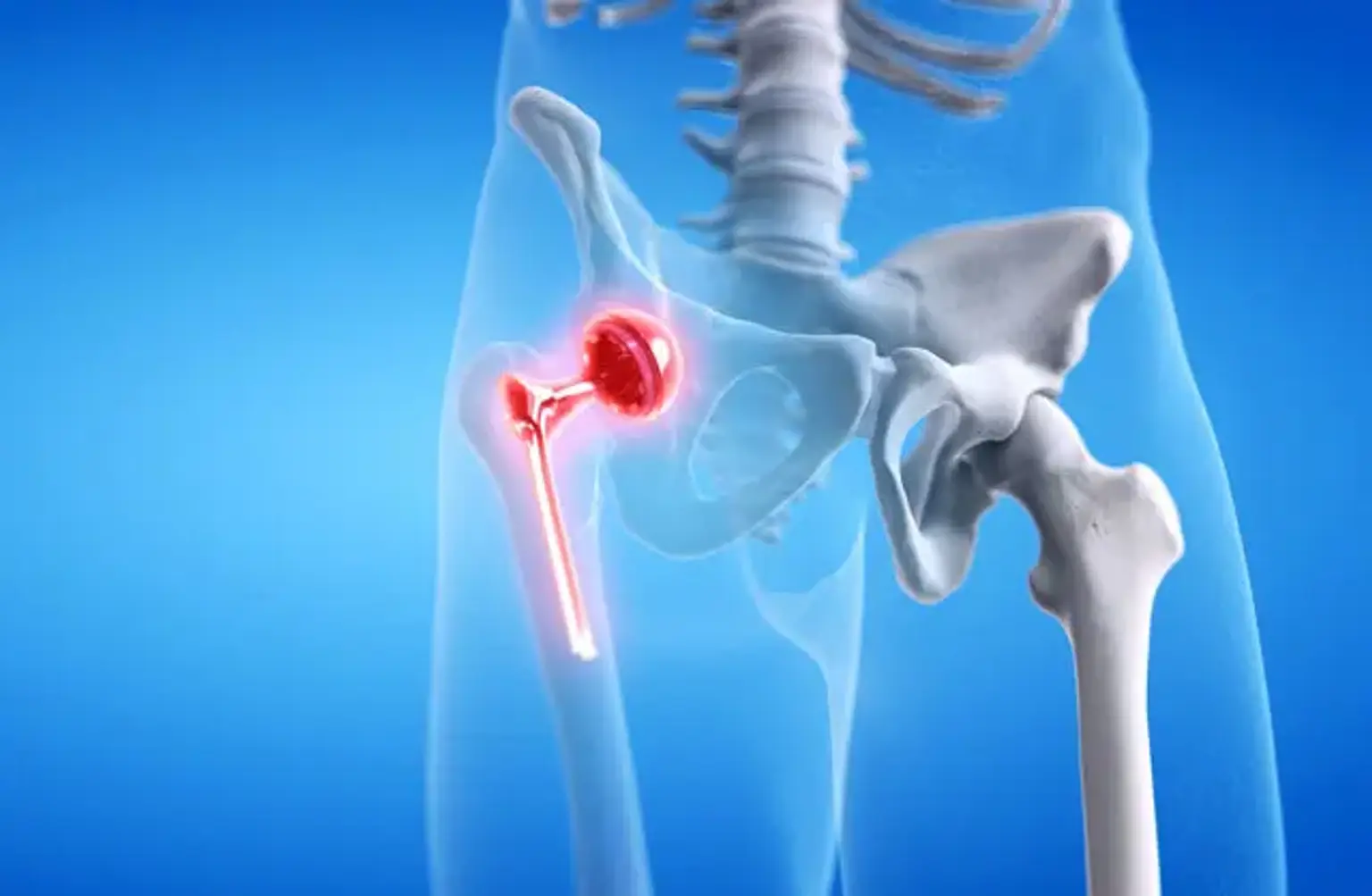
Arthroplasty, also known as joint surgery, is a surgical procedure to correct and restore joint function. During this procedure, the surgeon can remove a section of the damaged or injured joint and replace it using metal, plastic, or a ceramic device.
Also, the surgeon can use various replacement prostheses as well as surgical techniques. This depends on your joint shape and size, age, activity level, weight, and general health.
Arthroplasty hip and knee replacement are usually the most prevalent forms that surgeons often perform. However, they can also conduct the procedure on other joints such as the elbow, ankle, wrist, and shoulder.