Asherman's Syndrome
Overview
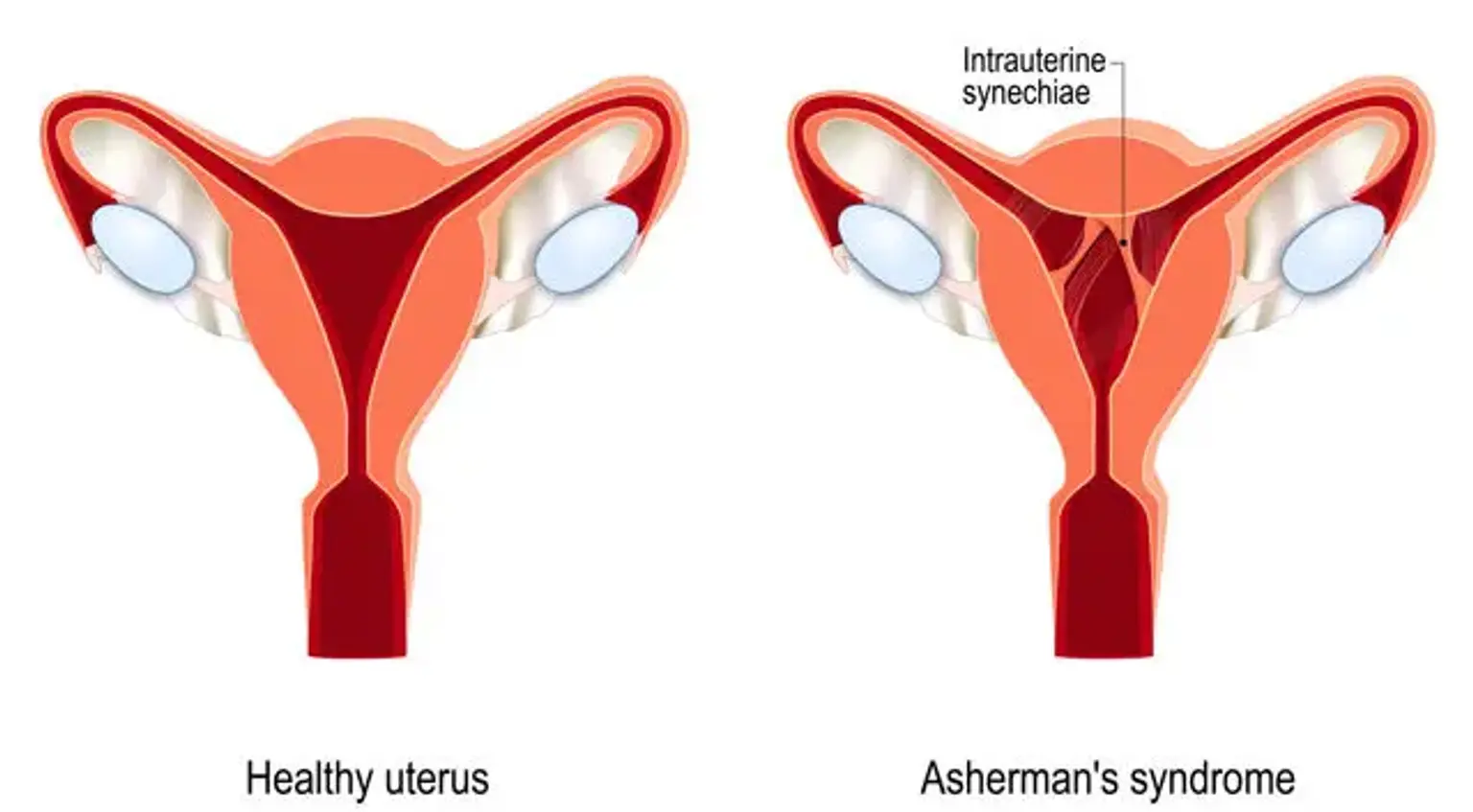
Asherman's syndrome is an uncommon, acquired uterine gynecological condition. It is distinguished by the bonding of scar tissue that borders the uterine walls, which reduces the volume of the uterine cavity. Intrauterine adhesions or synechiae can form as a result of surgical scraping or cleaning of tissue from the uterine wall (dilatation and curettage [D and C]), endometrial infections (e.g., genital TB), or other reasons.
Asherman's syndrome can range from severe (when more than 75% of the uterine front and back walls fuse together) to moderate and mild, where only tiny sections of the uterine wall fuse together. Depending on the severity of the condition, patients may have a variety of symptoms, including decreased menstrual flow, increased cramping and abdominal discomfort, ultimate cessation of menstrual periods (amenorrhea), and, in some women, infertility.
Hysteroscopic surgery, as well as preventative (Foley catheter) and restorative treatments, are currently available as therapy alternatives (hormone treatment). Newer approaches, including as stem cell therapy, are also being investigated to treat severe instances of Asherman's syndrome.