Atherosclerosis
Overview
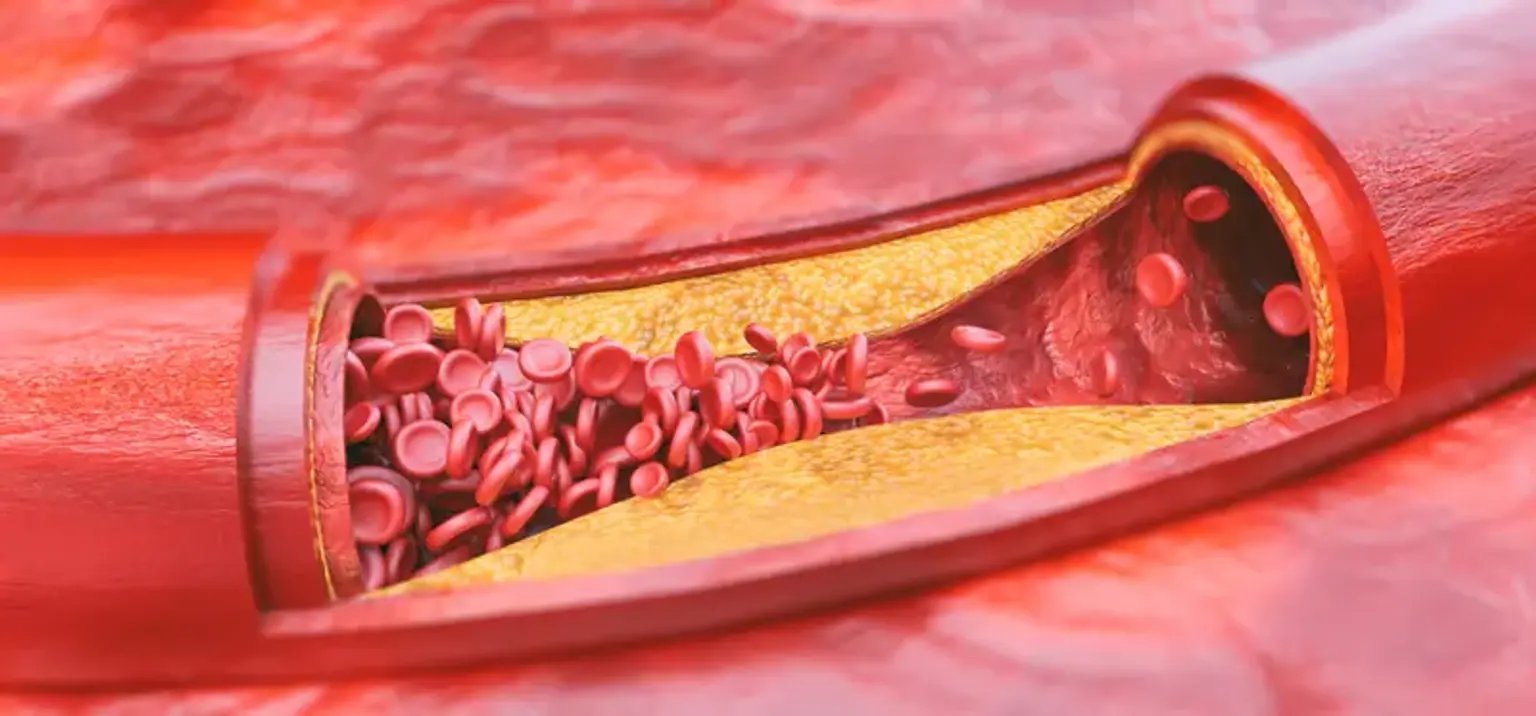
Atherosclerosis is the accumulation of plaque (fatty deposits) in your arteries. The blood artery wall thickens as plaque accumulates. This narrows the artery's lumen, limiting blood flow. This reduces the quantity of oxygen and other nutrients that reach the body.