Bile duct stones
Overview
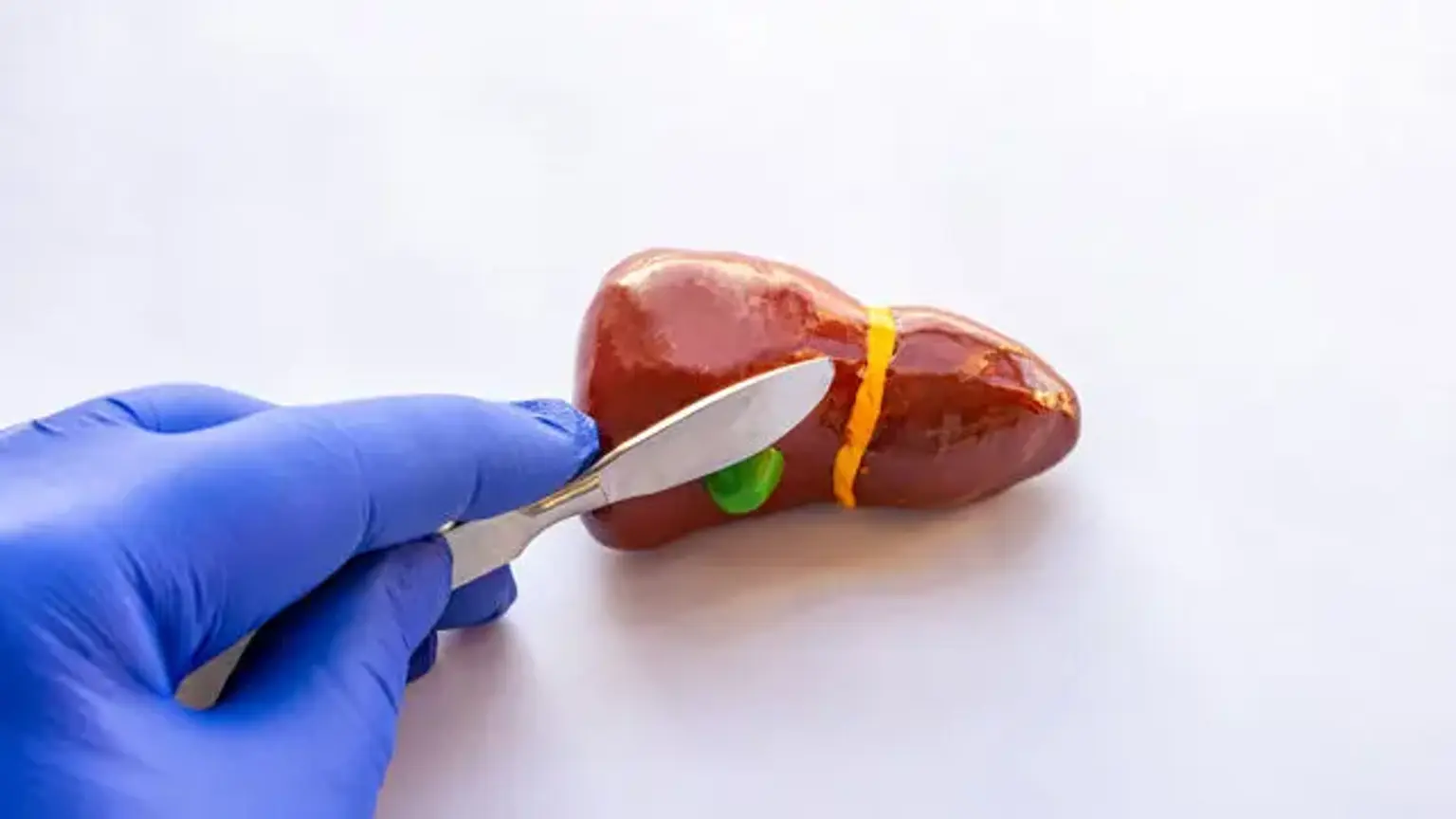
The presence of one or more gallstones in the common bile duct is referred to as bile duct stones (Choledocholithiasis). This often happens when a gallstone moves from the gallbladder into the common bile duct. Cholangitis, jaundice, and direct detection of stones with ultrasonography are the greatest indicators of the existence of common bile duct stones (CBDS).