Bowel Surgery
Overview
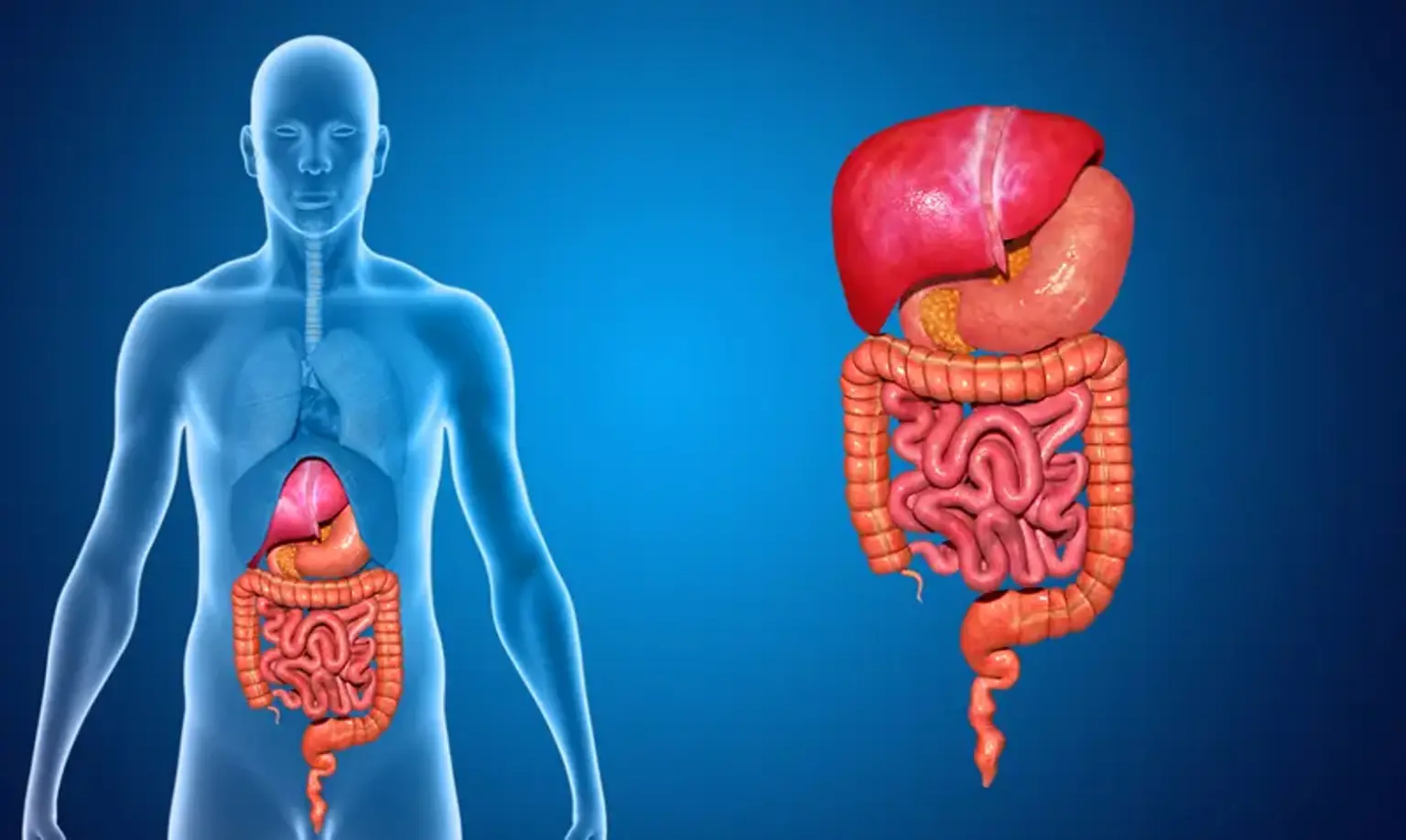
The bowel is the digestive system's lowest section. The digestive system is sometimes referred to as the gut or the gastrointestinal tract (or the GI tract or GIT for short). The bowel travels from the stomach to the anus. It is a muscular tube that is hollow. It breaks down all of the food we ingest into nutrients that the body can utilize. It also eliminates any solid waste stuff from the body in the form of poo (also called feces or stools).