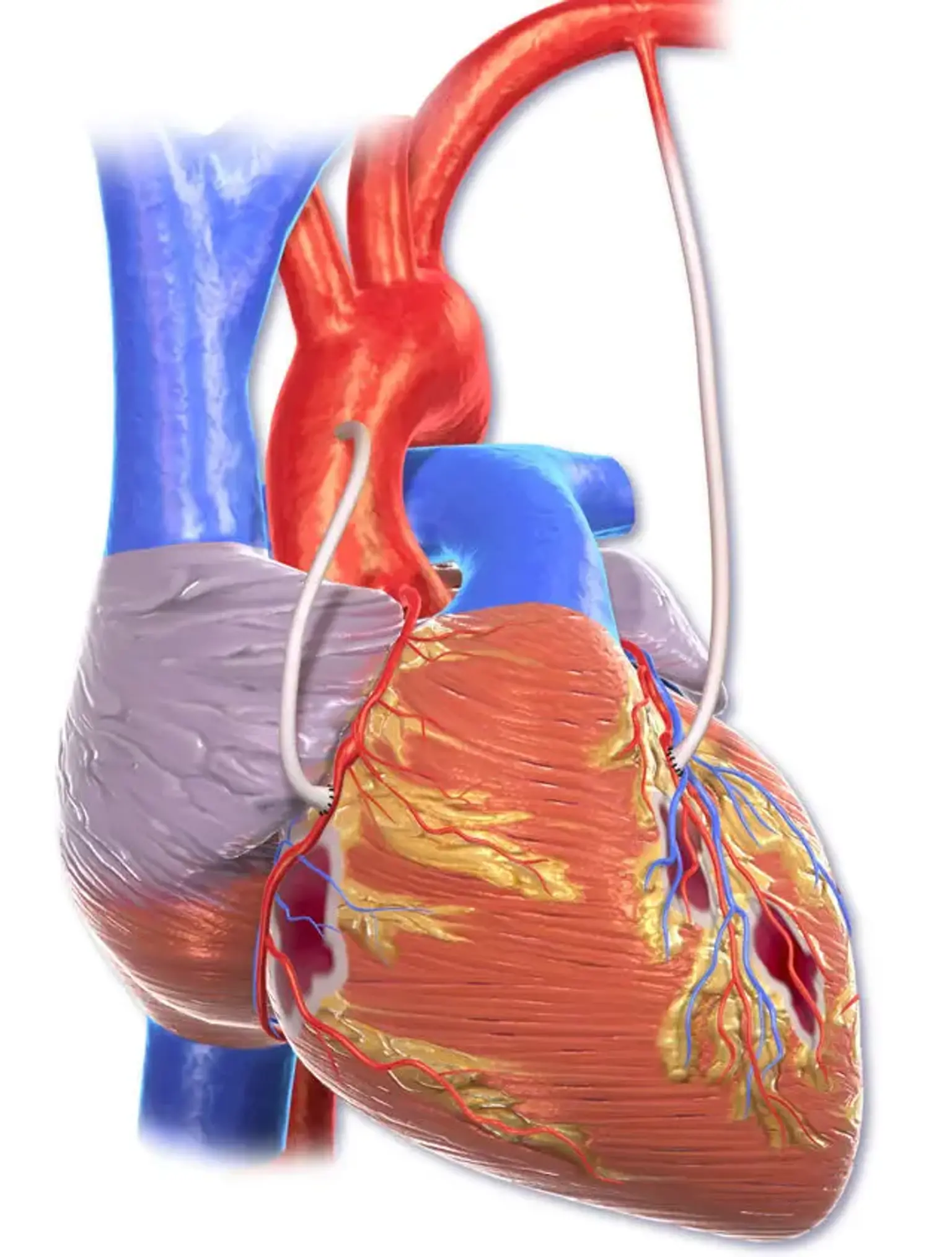
Coronary Artery Bypass Graft (CABG)
Overview
CABG is a significant surgical procedure in which atheromatous obstructions in a patient's coronary arteries are bypassed using harvested venous or arterial conduits. The bypass restores blood flow to the ischemic myocardium, restoring function and viability and alleviating anginal symptoms.
Almost 400,000 CABG operations are conducted each year, making it the most regularly performed major surgical surgery; however, surgical trends have shifted as alternate choices such as medical therapy and percutaneous coronary intervention (PCI) have become more popular.