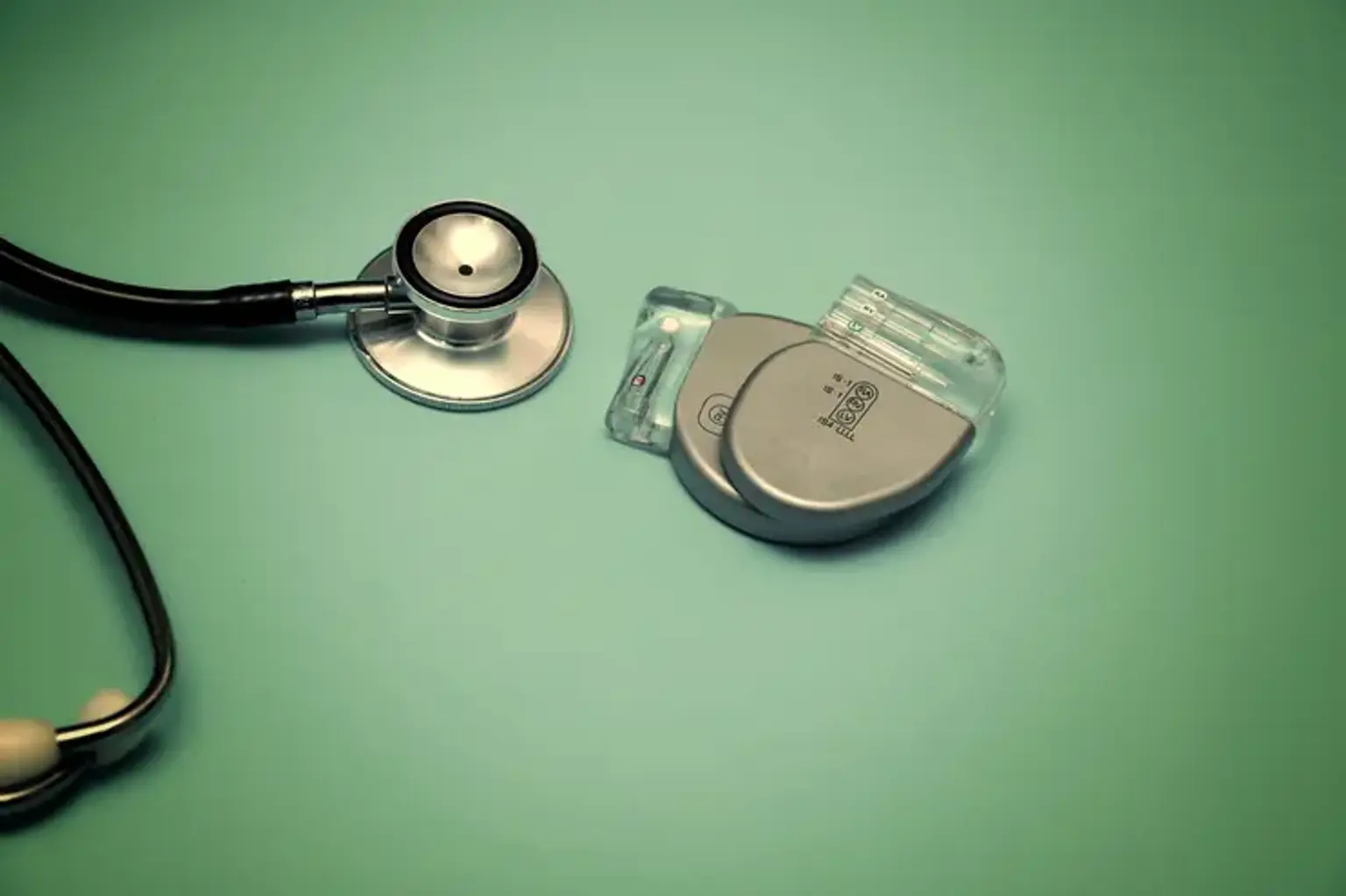
Cardiac Resynchronization Therapy (CRT)
Overview
Systolic heart failure is a serious concern in the United States today, with 550,000 new cases diagnosed each year, contributing to 287,000 fatalities. While pharmacologic treatment has significantly improved outcomes in individuals with systolic heart failure, hospitalizations continue to rise and remain a significant financial burden. Cardiac resynchronization treatment attempts to restore mechanical synchrony by electrically stimulating the heart in a coordinated fashion.