Cerebral aneurysm
Overview
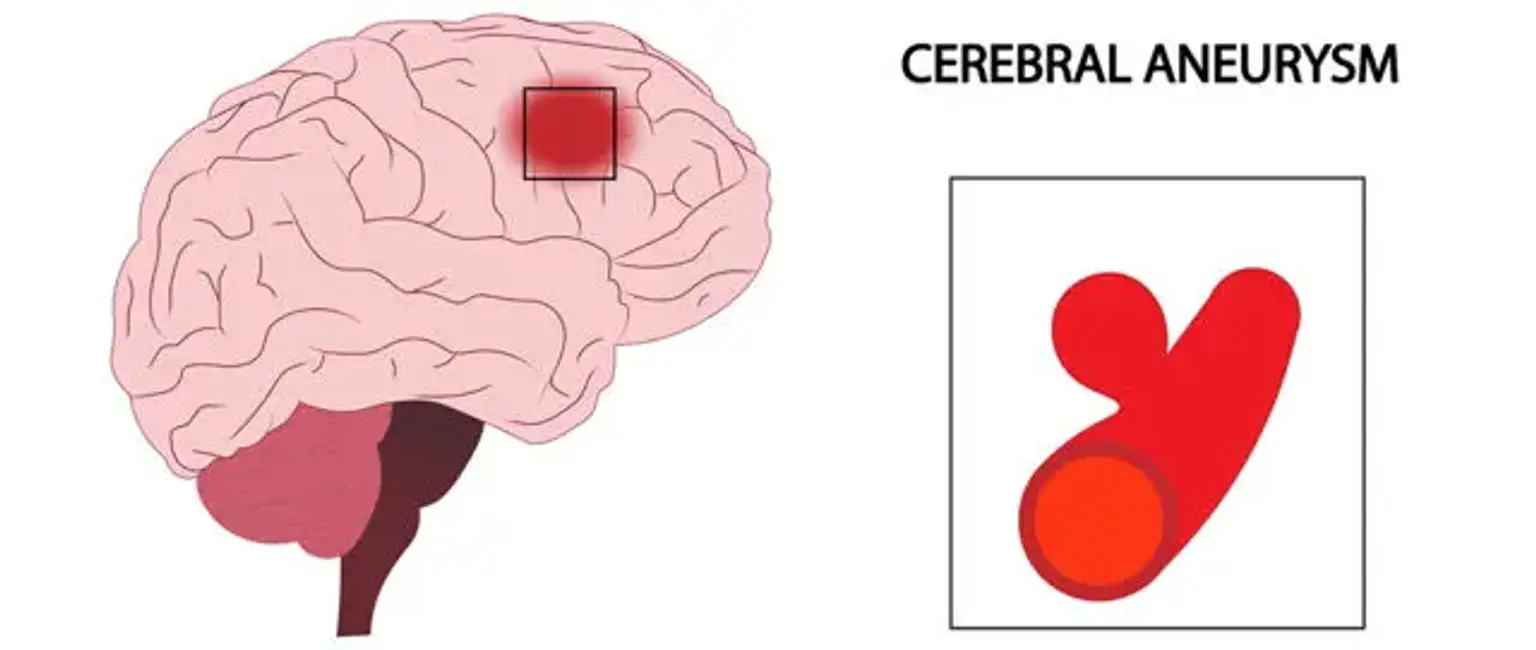
A cerebral aneurysm is a ballooning that occurs as a result of a weak spot in the wall of a blood artery in the brain. If the brain aneurysm grows in size and the blood artery wall gets too thin, the aneurysm will rupture and leak into the brain space.