Cervical Disc Replacement
Overview
Non-spinal diseases such as rotator cuff tears, tennis elbow, and carpal tunnel syndrome can all cause or contribute to arm and neck pain. The problem for certain people is frequently with the spinal column and nerves in the neck, known as the cervical spine. A ruptured or bulging disc that pushes on these spinal nerves is one of the most prevalent ailments. Previously, the sole treatment was to remove the cervical disc and fuse the vertebrae in the neck together. This was frequently done with bone from the "hip" or the iliac crest. This required patients to have an additional procedure, which was frequently more painful than the neck surgery.
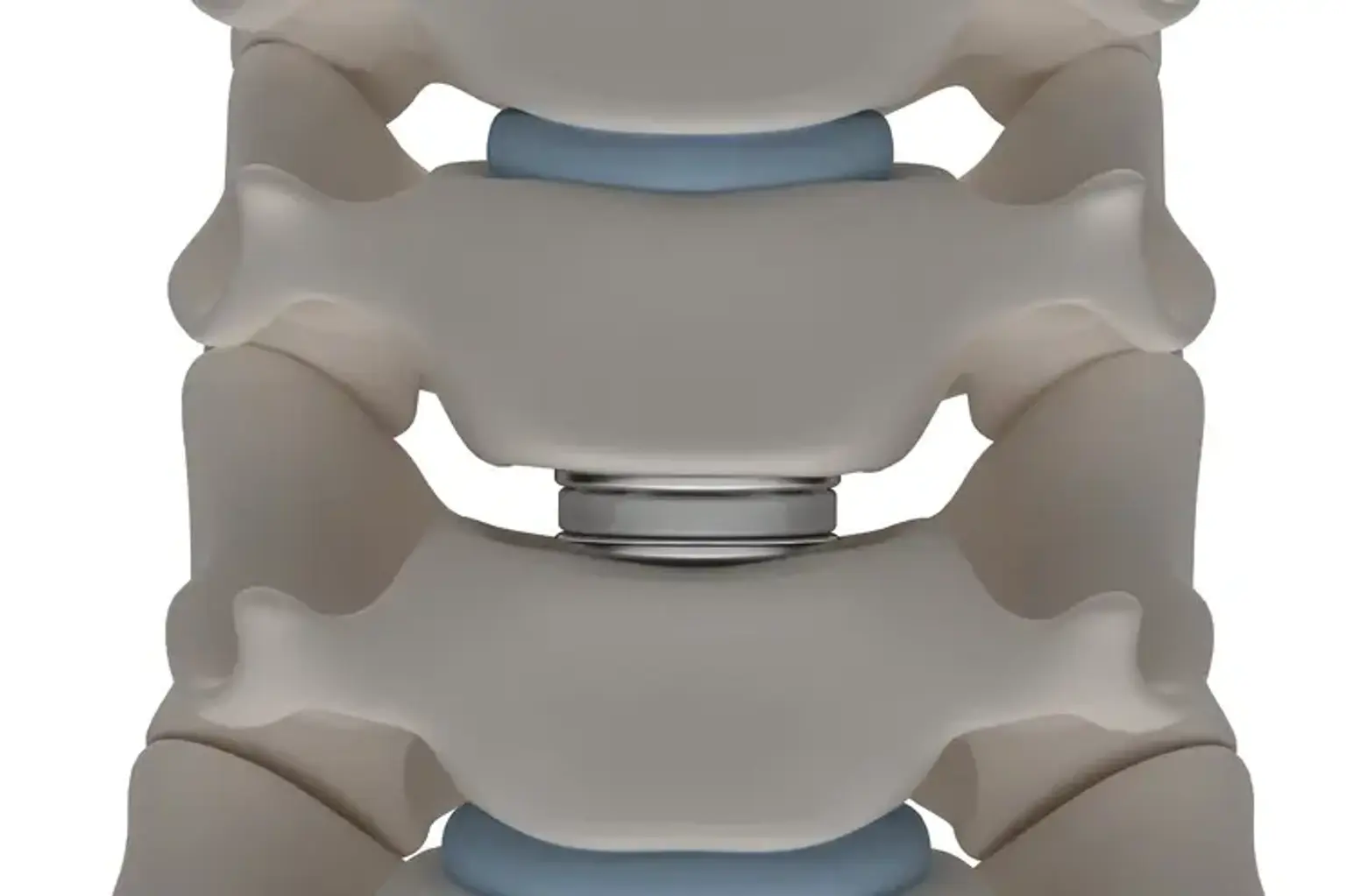
Several prosthetic cervical discs, on the other hand, have been created and are now accessible as a surgical alternative to address cervical disc abnormalities that cause persistent neck pain and other symptoms such as arm discomfort or paralysis.