Chronic lymphocytic leukemia
Overview
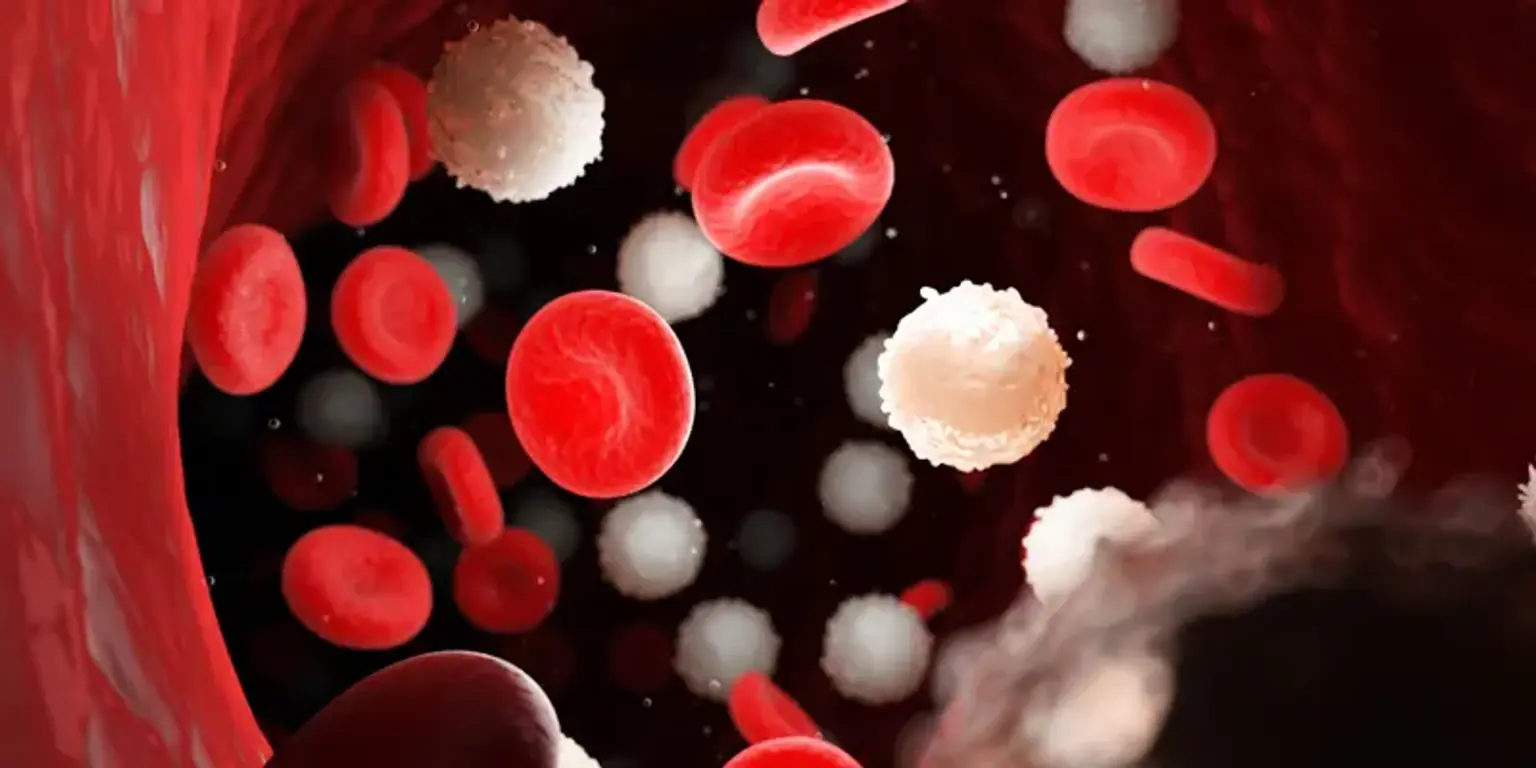
Chronic lymphocytic leukemia (CLL) is a blood and bone marrow malignancy. CLL affects white blood cells known as lymphocytes. It takes a long time to develop. It is the most prevalent adult leukemia in Western nations, accounting for 25 to 30 percent of all leukemias in the US. There are several varieties of leukemia, and the therapy you require is determined by which type you have.