Chronic obstructive pulmonary disease
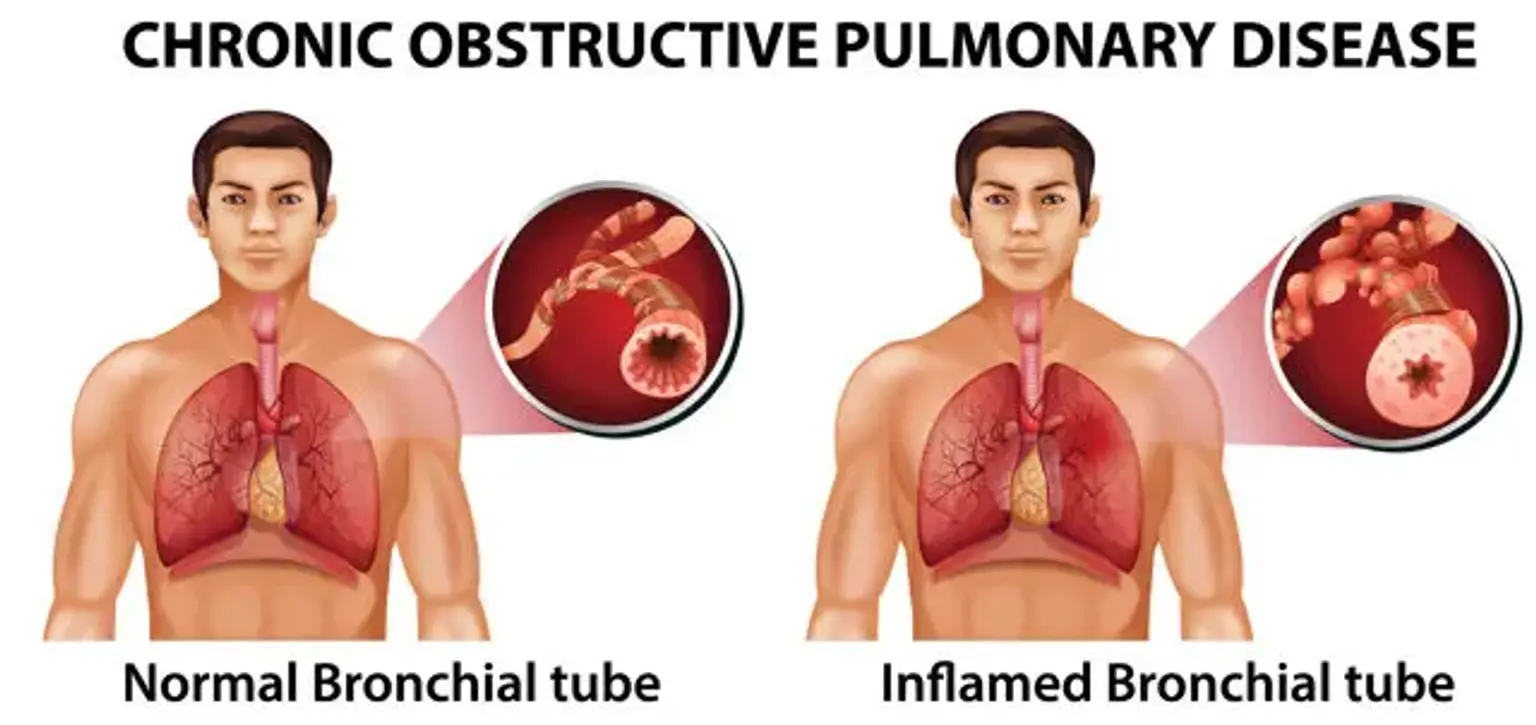
Chronic obstructive pulmonary disease (COPD) is a group of illnesses that leads to airflow obstruction and breathing issues. Chronic bronchitis and emphysema are the most common disorders that can lead to COPD. If you've been diagnosed with COPD, you may have one or both of these respiratory illnesses or symptoms of the two. COPD can progress slowly, making breathing increasingly difficult with time.
COPD is generally treatable, even though it is a progressive condition that worsens with time. Most patients with COPD can obtain good symptom management and quality of life with effective control and a lower chance of developing other illnesses.