Cirrhosis
Overview
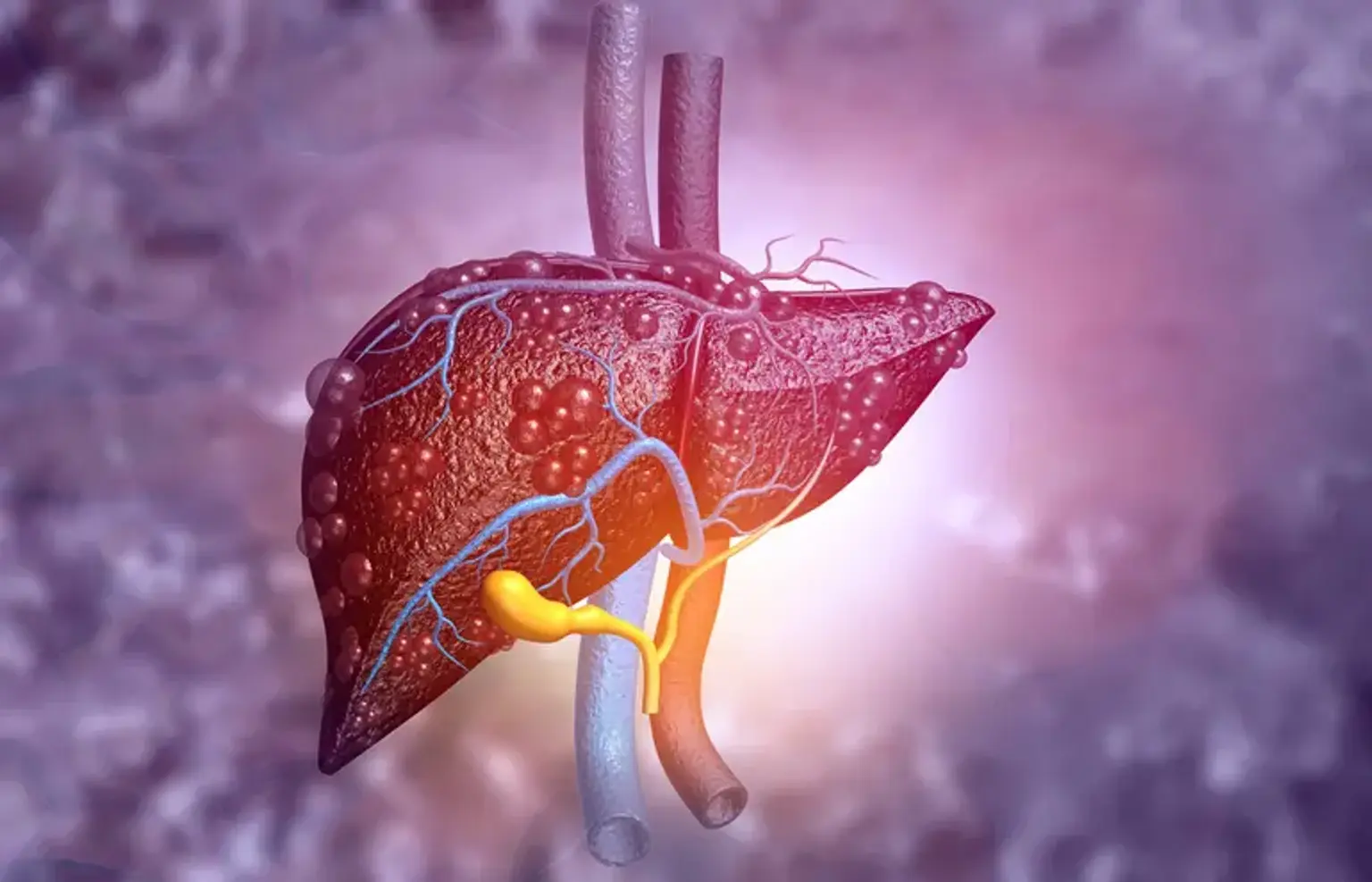
Cirrhosis is a condition in which your liver is scarred and permanently damaged. Cirrhosis has many signs and symptoms, such as fatigue and severe itchy skin. Doctors diagnose cirrhosis based on your medical history, a physical exam, and the results of tests. Doctors do not have specific treatments that can cure cirrhosis. However, they can treat many of the diseases that cause cirrhosis. Treating the underlying causes of cirrhosis may keep your cirrhosis from getting worse and may help prevent liver failure.