Coronary Angiography
Overview
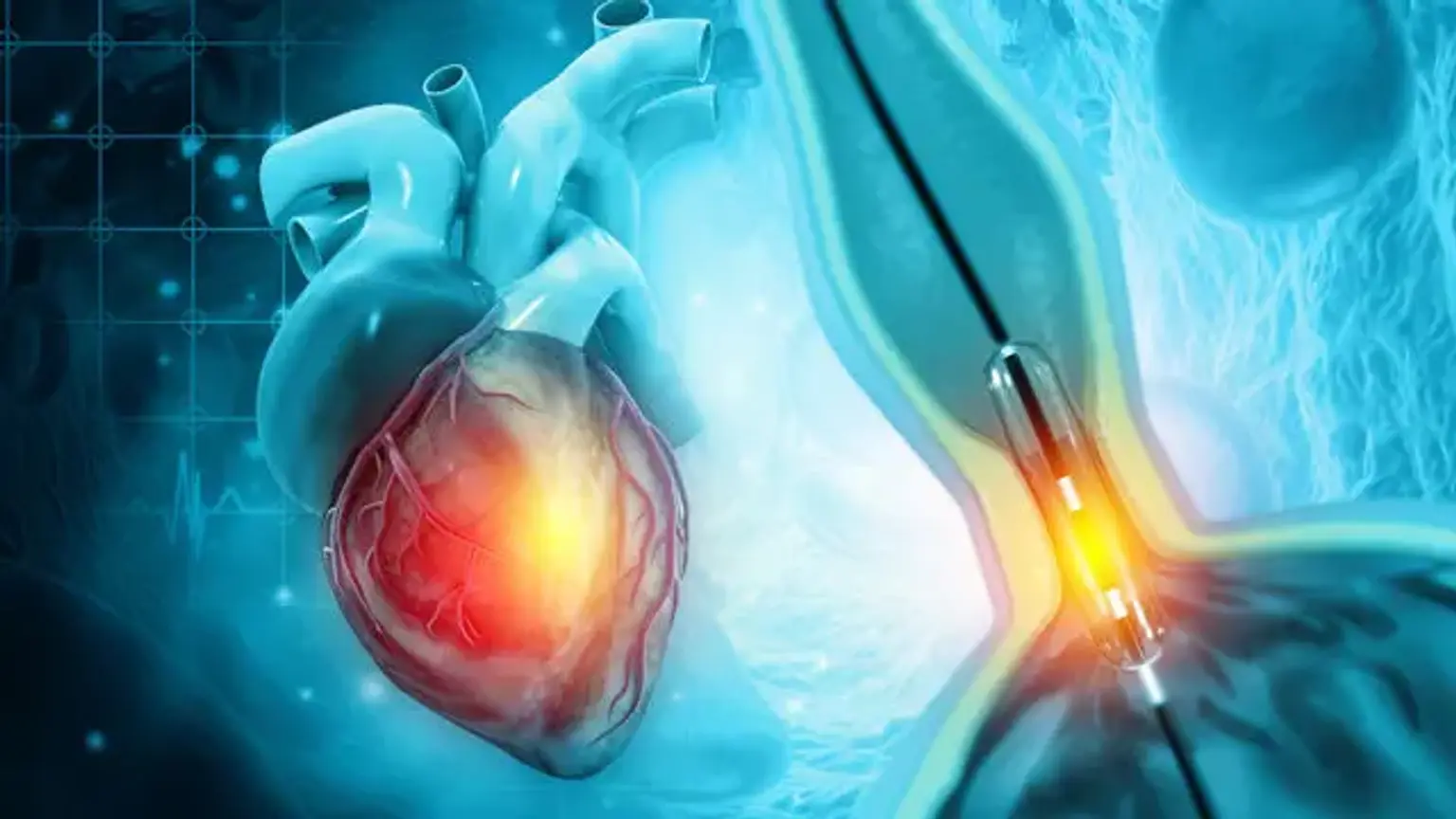
The anatomical and structural characteristics of the circulatory system, including the heart chambers, are identified by angiography. Angiography was originally utilized for structural diagnosis of intravascular diseases, but it has now been broadened to include functional evaluation and therapy choices.
Coronary angiography and cardiac catheterization are vital diagnostics for detecting and quantifying coronary artery disease, identifying valvular and other structural anomalies, and measuring hemodynamic parameters. The risks and consequences connected with these treatments are related to the patient's coexisting diseases as well as the operator's expertise and discretion.