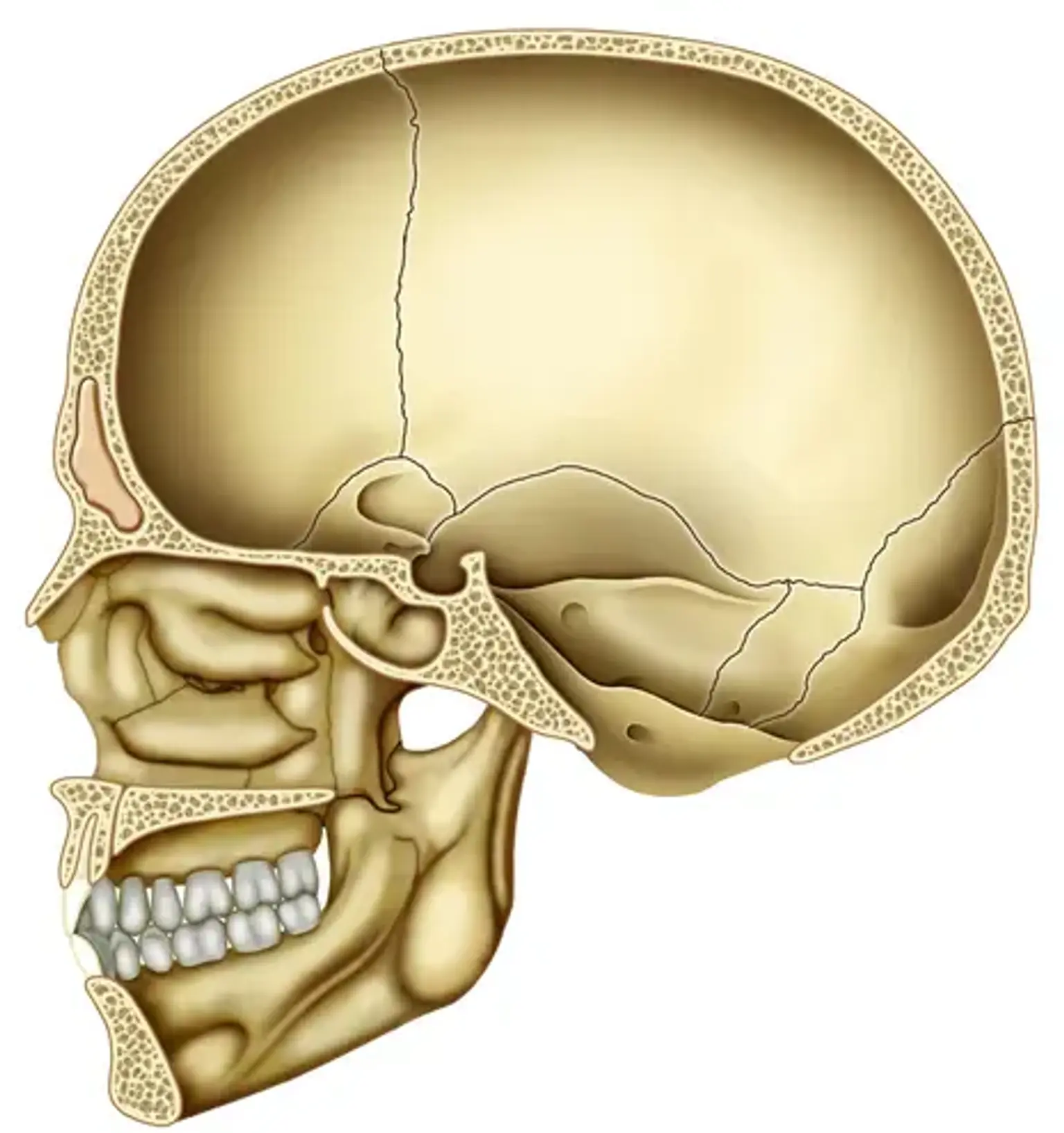
Cranial Base Disease
Every nerve that connects the brain to the rest of the body must pass via the cranial base, a tiny but incredibly complex region at the base of the skull. You may encounter neurological issues like headaches, facial pain, blurred vision, dizziness, or seizures if you have a cranial base disease. When the tumor has gotten big enough to press against the brain or the nerves, these symptoms frequently appear.