Craniotomy
Overview
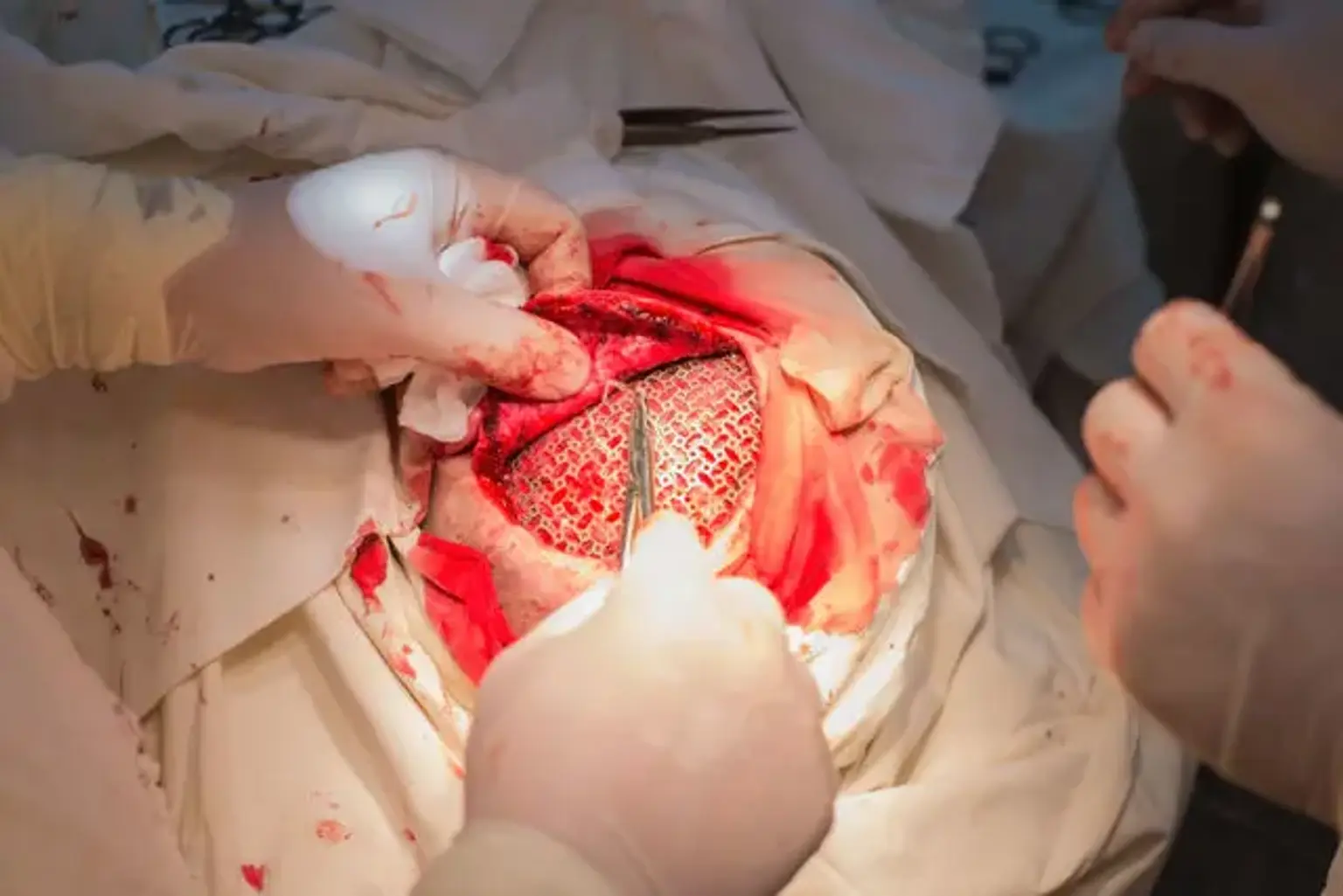
A craniotomy is a surgical procedure that involves temporarily removing a portion of the skull in order to expose the brain and perform an intracranial surgery. Brain tumors, aneurysms, arterio-venous malformations, subdural empyemas, subdural hematomas, and intracerebral hematomas are among the most frequent disorders that may be treated using this method.
Specialized tools and equipment are used to remove the bone flap, which is a portion of bone. The bone flap is removed temporarily, held at the surgical instrument table, and then replaced when the brain operation is completed.
The bone can be discarded, kept in the abdomen subcutaneous area, or cryopreserved under cold storage conditions in some situations, depending on the etiology and indication for the treatment. The technique is known as a craniectomy if the bone flap is discarded or not put back into the skull during the same operation.