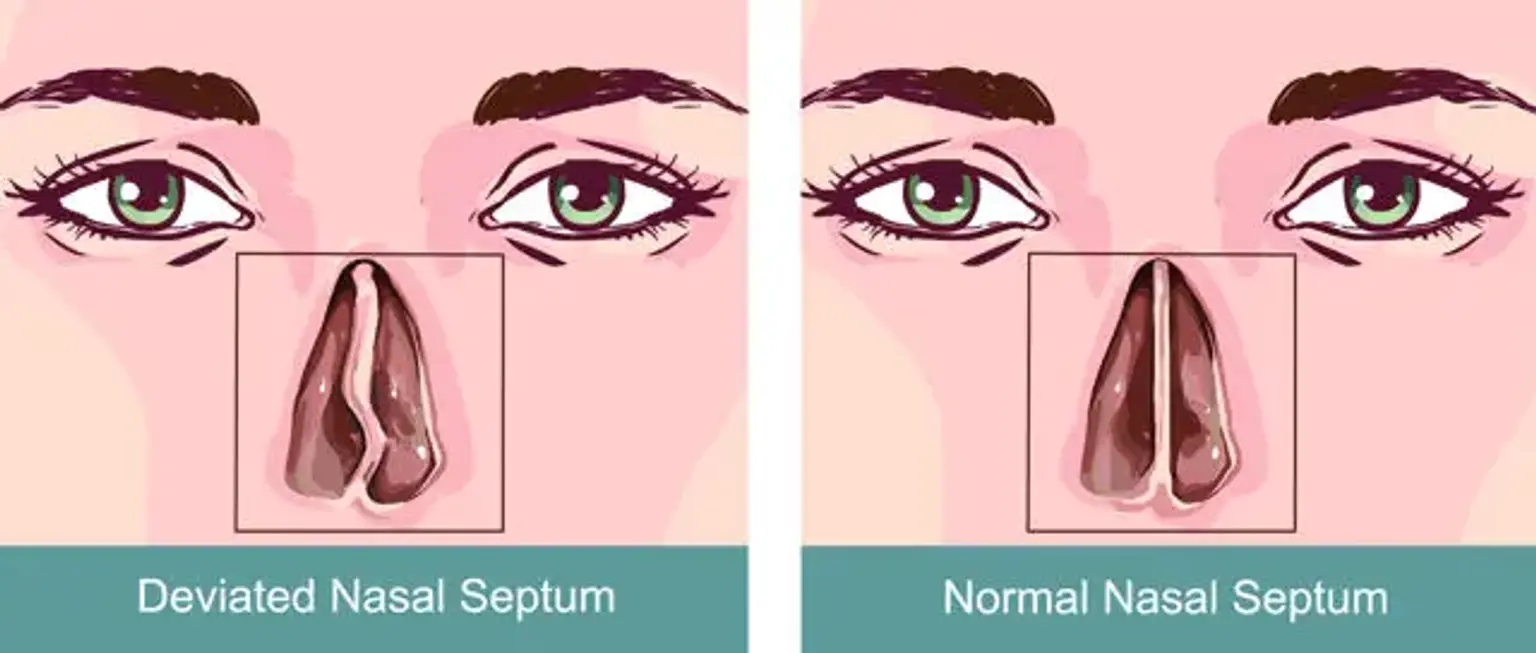
Deviated septum
The septum is the nose's principal supporting structure, providing support to the dorsum, columella, and nasal tip. It also divides the nasal cavity, resulting in two unique nasal airways that allow for warming, humification, and turbulent air movement. A septum deviation can lower the cross-sectional area of the nasal valve, resulting in airway obstruction.
This can cause nasal obstruction and, in rare cases, aggravate the symptoms of obstructive sleep apnea. Epistaxis, headaches, and face discomfort can be caused by bony spurs caused by a deviated nasal septum.