Introduction
Ear disorders can significantly affect a person’s quality of life, leading to issues like hearing loss, discomfort, and emotional distress. Ear health is crucial, as the ears play an essential role in communication, balance, and overall well-being. While many ear disorders can be treated, a specialized procedure known as ear volume restoration is gaining popularity, especially in countries like Korea. This procedure helps restore both the physical appearance and functionality of the ear, which may be compromised due to injury, aging, or disease.
Why is ear disorder treatment important? Treating ear disorders not only improves hearing but also enhances one’s self-esteem and social interactions. This article will explore various ear treatment options, including innovative volume restoration methods, and discuss their effectiveness and popularity, particularly in Korea.
Causes of Ear Disorders
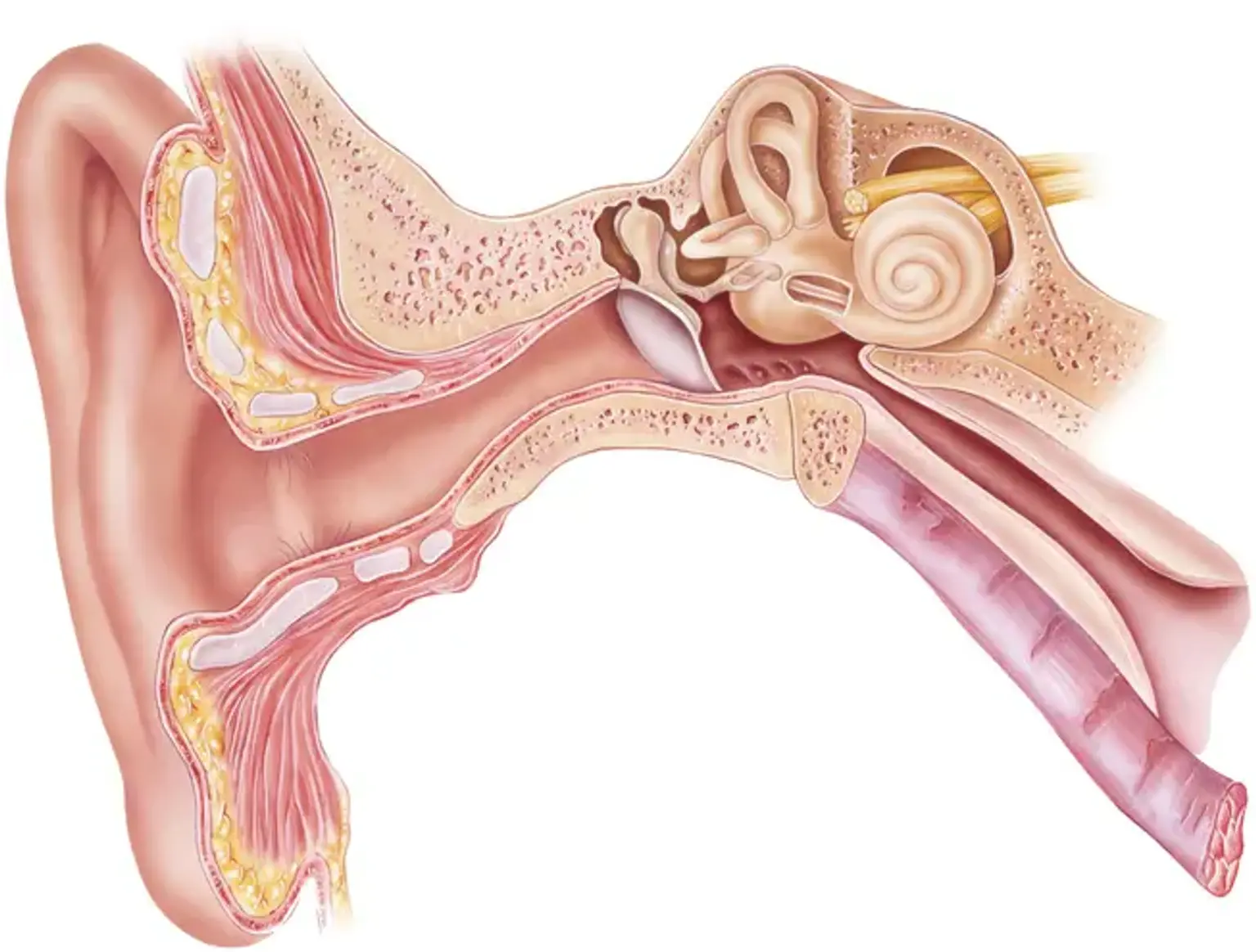
Ear disorders can arise from a variety of factors, including chronic ear conditions like infections, trauma, and genetic predisposition. Hearing loss, in particular, is a leading concern and can stem from both age-related degeneration and environmental factors such as prolonged exposure to loud noises.
Key Causes of Ear Disorders:
Aging: As people age, hearing tends to degrade, often leading to volume loss in the ear.
Infections: Middle ear infections and other conditions can damage the ear's internal structure.
Trauma: Accidents or injury to the ear can affect its volume and function, requiring restoration.
Noise Exposure: Chronic exposure to loud sounds can cause permanent damage to ear cells.
Volume loss and hearing loss are often interconnected. When ear volume is diminished, it can impact the ear's ability to transmit sound properly, leading to hearing difficulties. For those suffering from hearing loss or ear deformation, treatments like ear volume restoration can be life-changing.