Endometrioma
Overview
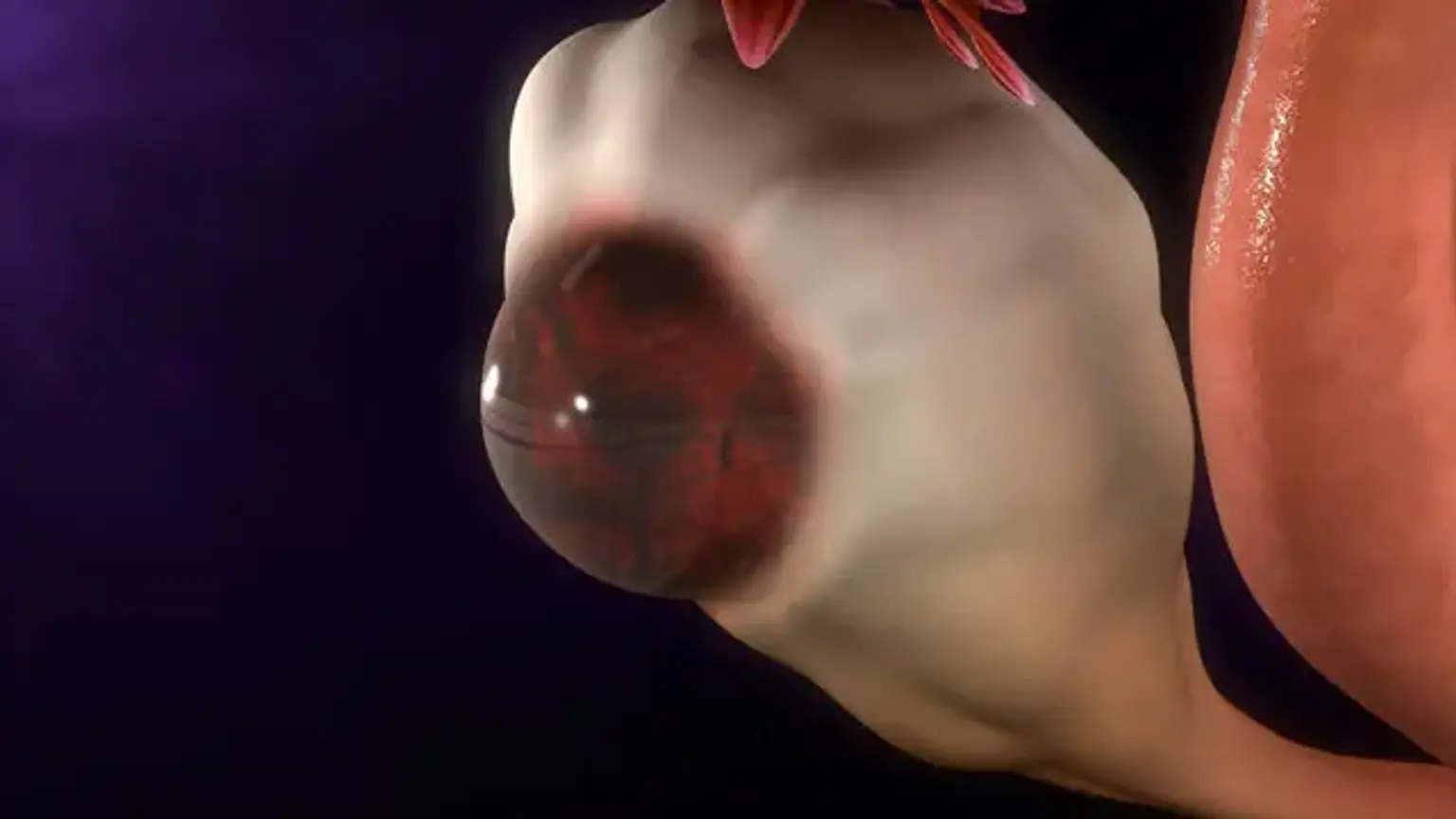
Endometriomas are cysts that grow on the ovaries and are sometimes known as "chocolate cysts" due to their dark hue. Endometrial tissue that forms on the ovaries causes these cysts. Endometrioma can develop in women with endometriosis.
Endometrioma symptoms include painful periods and profuse menstrual flow. Expectant management, medicinal and/or surgical therapy, and in vitro fertilization are all alternatives for treatment. The choice of therapy is primarily determined by the related symptoms.