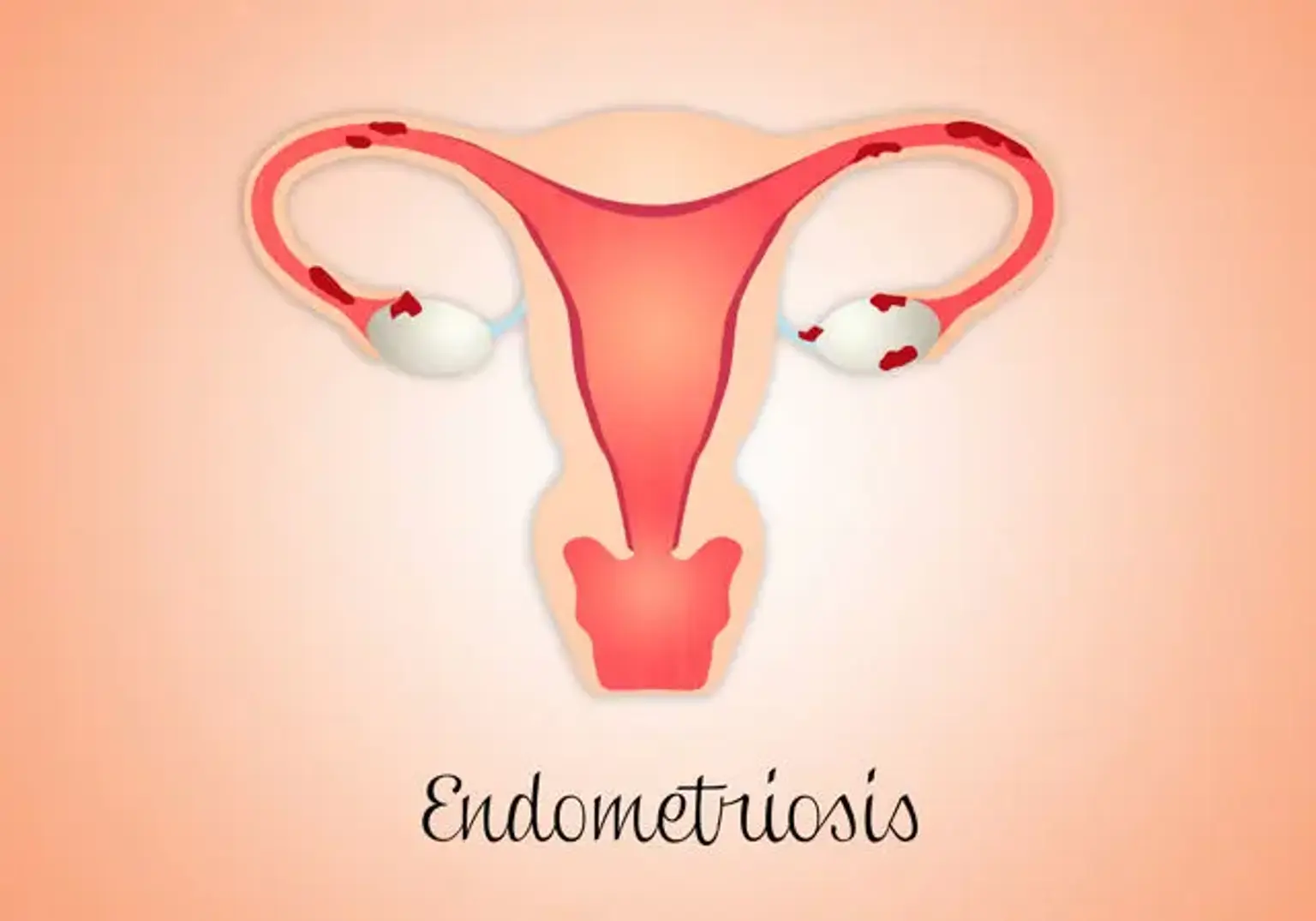
Endometriosis
Endometriosis is a gynecological disorder that affects about 10 percent of females. It’s whereby the tissue similar to that which lines the uterus develops outside the uterus. It’s typically a painful condition that mostly affects the fallopian tubes, ovaries, and the tissue that lines the pelvis. In rare cases, the endometrial tissue can spread away from the pelvic organs.
The endometrial tissue that develops outside the uterus is referred to as an endometrial implant. The hormonal alteration of the menstruation cycle alters the misplaced tissue, making the region painful and inflamed. Hence, the tissue grows, thickens, and eventually breaks down. With time, the broken tissue is stuck and has nowhere to shift; instead, it gets trapped within the pelvis.