Introduction
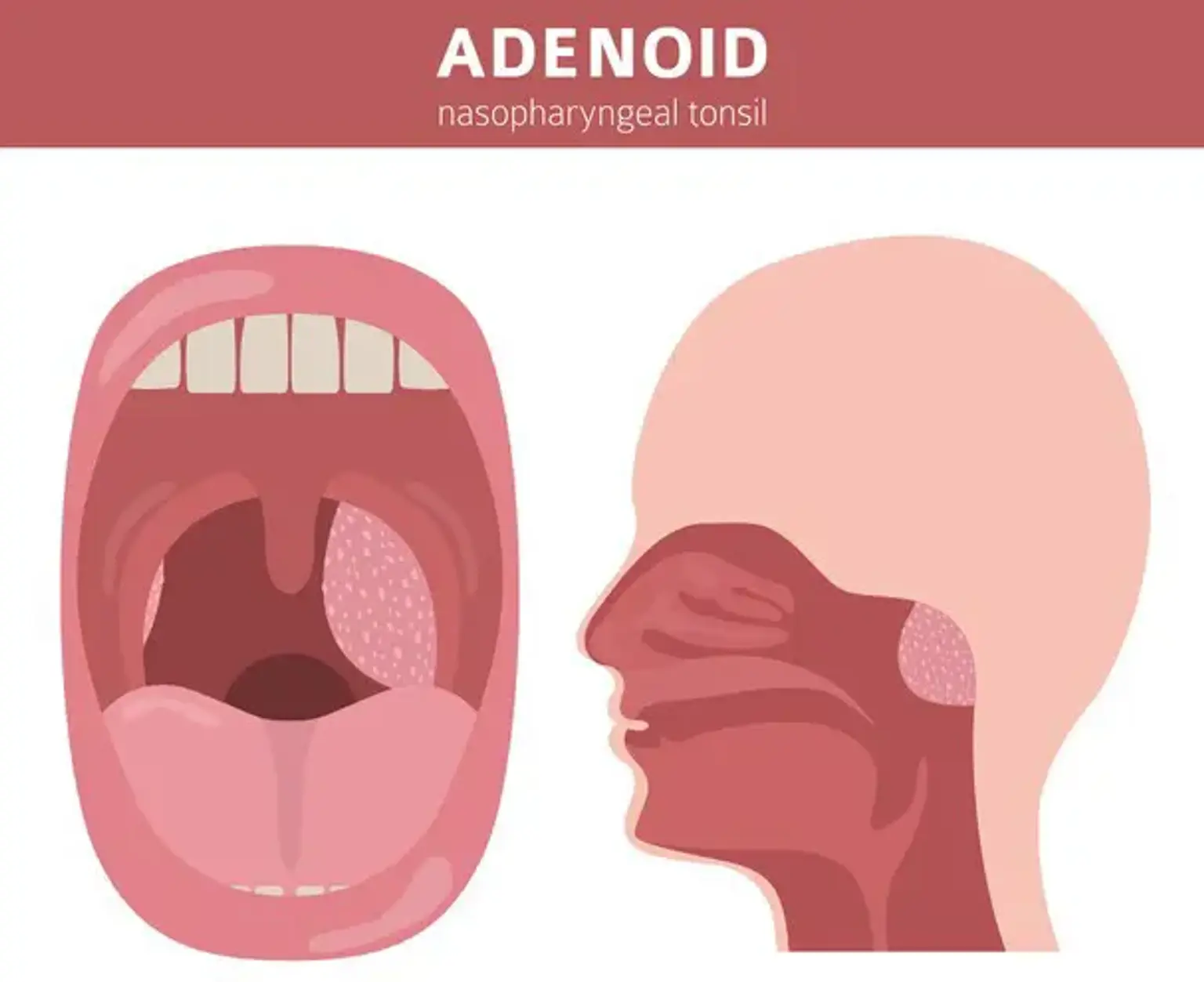
Endoscopic adenoid surgery, or endoscopic adenoidectomy, is a modern, minimally invasive procedure used to remove enlarged adenoid tissue from the back of the nasal passage. Traditionally, adenoidectomy involved a blind removal method using a curette or suction, which could cause complications.
The endoscopic approach, however, offers a clearer view, reduced risks, and a faster recovery time, making it a preferred option for many patients, especially children. This technique not only improves surgical precision but also minimizes post-operative complications, ensuring a smoother experience for patients.
Why Choose Endoscopic Adenoid Surgery?
The shift to endoscopic adenoidectomy has transformed the way the procedure is performed, offering significant advantages over traditional methods:
Precision: The use of an endoscope allows surgeons to view the adenoids clearly, ensuring a complete and accurate removal.
Reduced Risks: Unlike traditional methods, which can lead to bleeding or damage to surrounding tissues, the endoscopic approach minimizes these risks.
Faster Recovery: Because it's less invasive, patients generally experience quicker healing times and less discomfort.
Additionally, endoscopic surgery is highly effective for both children and adults, addressing conditions like sleep apnea, snoring, and chronic ear infections with improved results.