Endoscopic Mucosal Resection
Overview
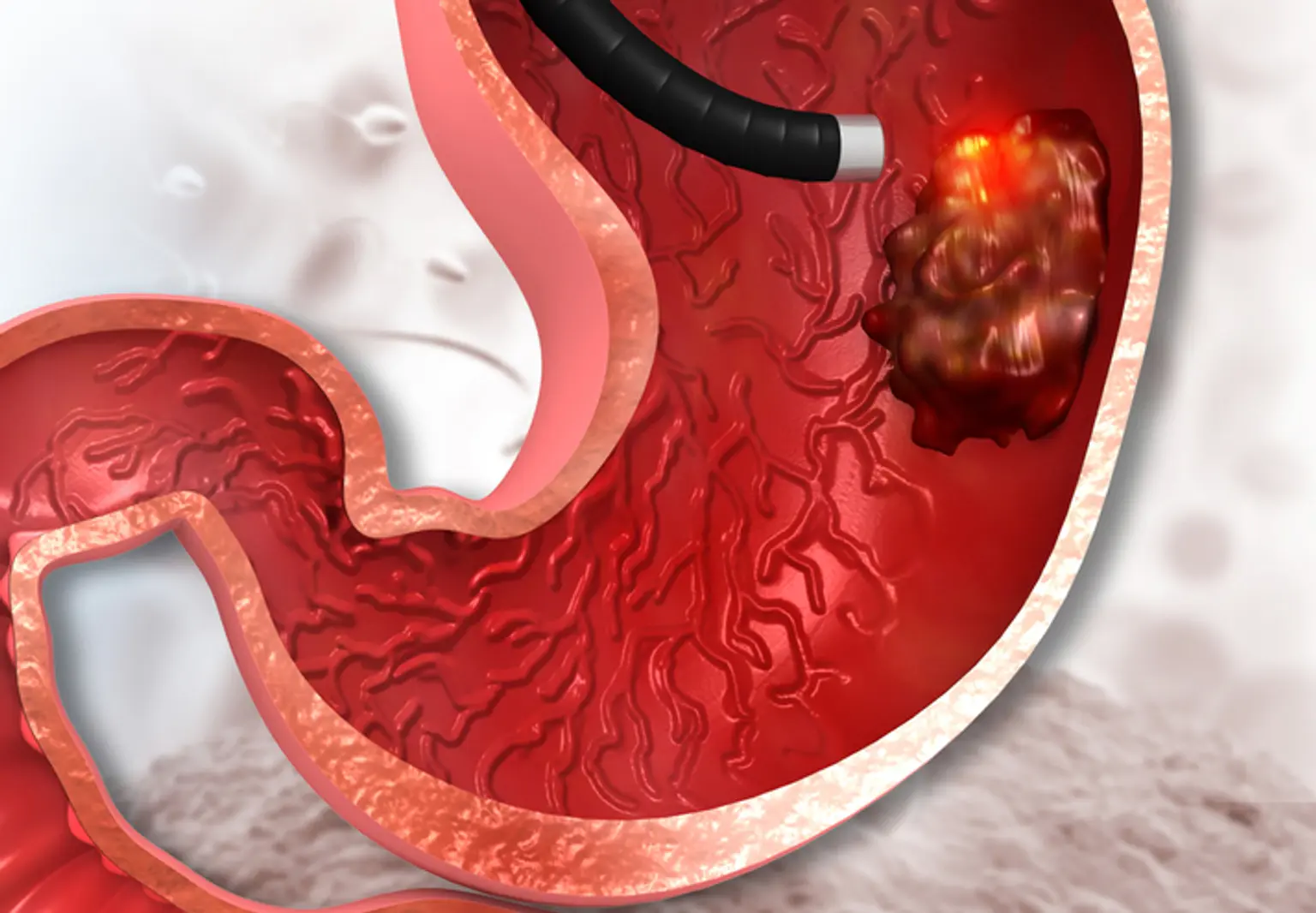
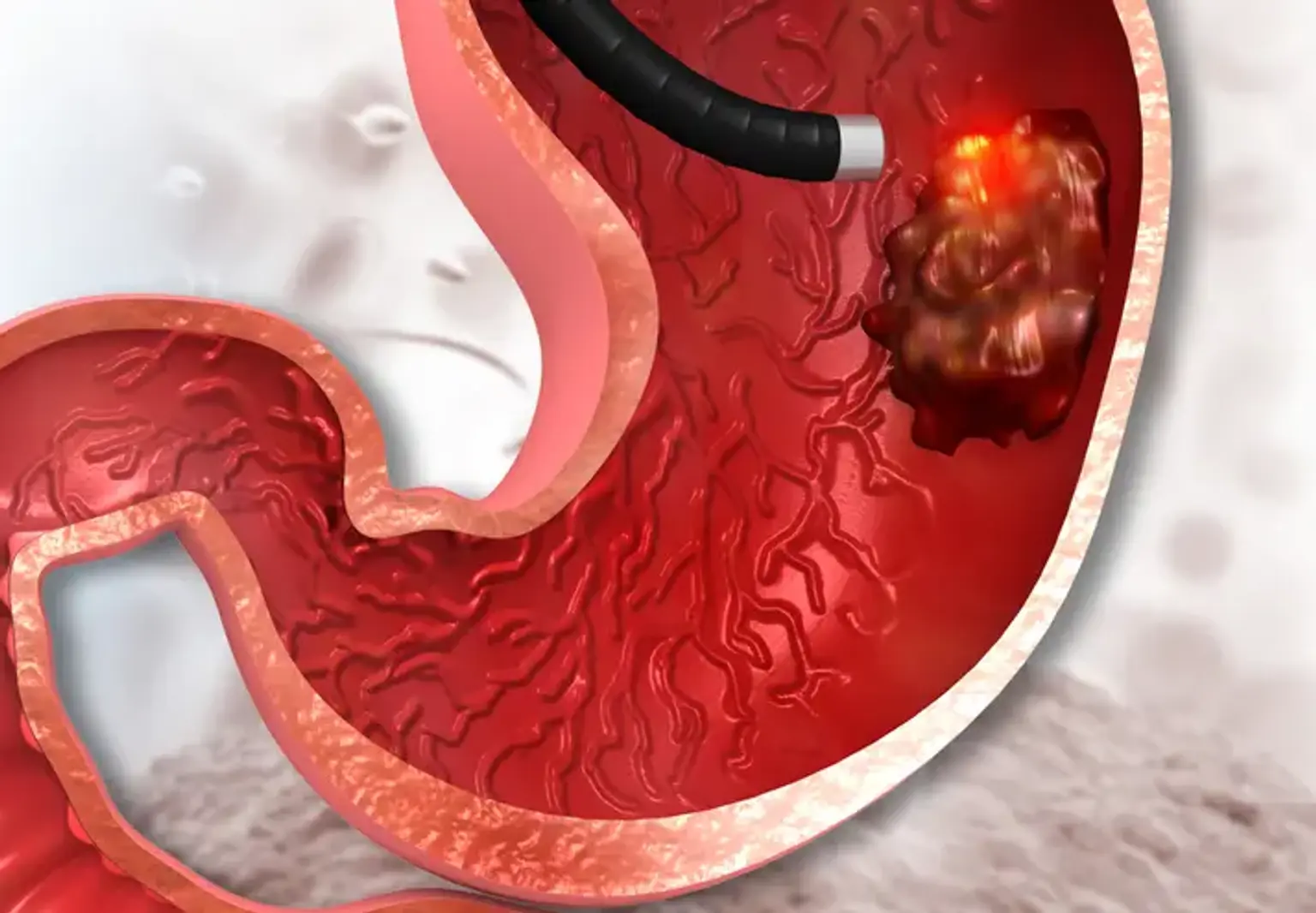
Endoscopic mucosal resection of the gastrointestinal tract (EMR) is a surgery used to remove precancerous, early-stage cancer or other abnormal tissues (lesions) from the digestive tract.
Endoscopic mucosal resection is carried out using a long, thin tube fitted with a light, video camera, and other devices. The tube (endoscope) is inserted down your throat during upper digestive tract EMR to reach an abnormality in your esophagus, stomach, or upper section of the small intestine (duodenum).
EMR is mostly used for treatment, but it is also utilized to gather tissues for diagnosis. If cancer is found, EMR can assist establish whether it has spread to areas beneath the digestive tract lining.