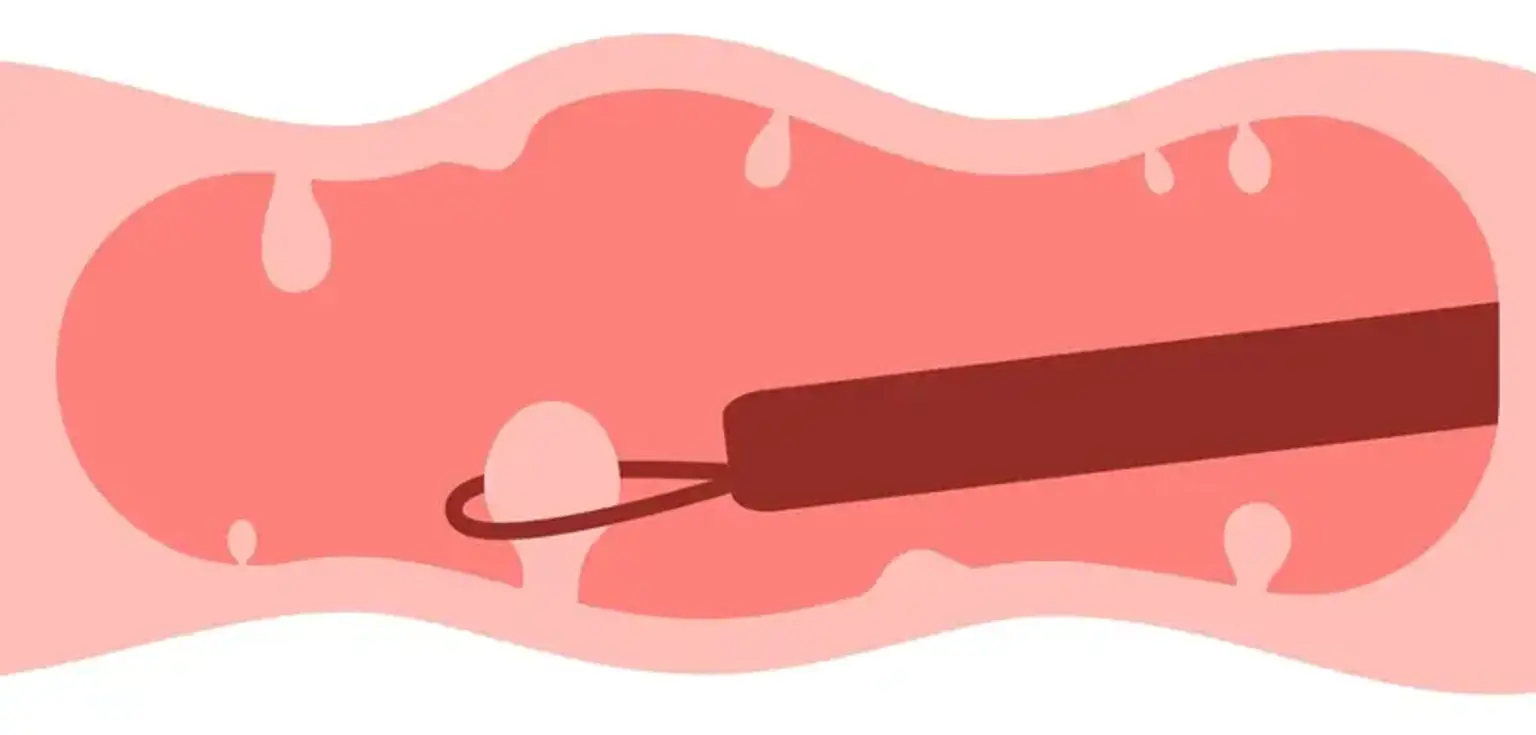
Endoscopic Polypectomy
Overview
In affluent nations, colorectal cancer is one of the most frequent malignancies. The adenoma to carcinoma sequence describes how most colorectal malignancies develop from colorectal adenomatous polyps. Colorectal adenomas can be detected and removed early to avoid the development of colorectal cancer. The great majority of these polyps are endoscopically removed. Endoscopic resection methods have advanced, allowing for more indications for endoscopic polypectomy, which can treat huge polyps, scarred lesions, and early malignancies.