Introduction
Uterine fibroids are non-cancerous tumors that develop in the wall of the uterus, affecting up to 80% of women by the age of 50. While many fibroids are symptom-free, others can cause significant issues, including heavy bleeding, pelvic pain, and even infertility. Traditional fibroid treatments have included invasive surgeries, but today, hysteroscopic fibroid removal offers a minimally invasive solution. This procedure has gained popularity globally due to its efficiency, reduced recovery time, and the ability to preserve fertility.
In this article, we’ll explore what hysteroscopic fibroid removal involves, the types of fibroids it treats, and the benefits it offers to patients.
What Are Uterine Fibroids?
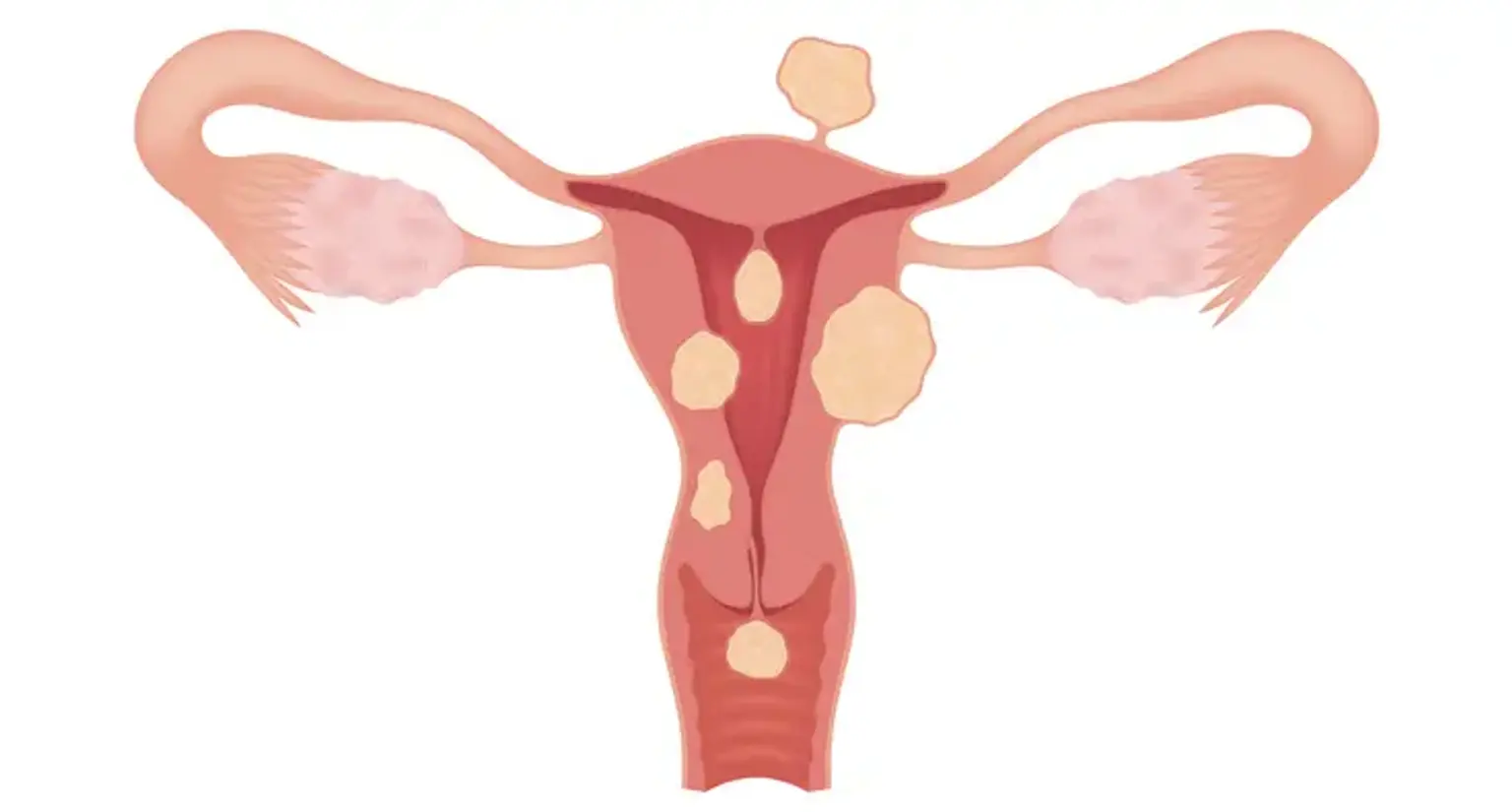
Uterine fibroids are benign growths made up of muscle and fibrous tissue that form in the uterus. These growths vary in size from tiny, undetectable nodules to large masses that can distort the shape of the uterus. Fibroids are categorized into three types:
Submucosal fibroids: Located just under the lining of the uterus, these fibroids can significantly affect menstruation and fertility.
Intramural fibroids: The most common type, growing within the muscular wall of the uterus.
Subserosal fibroids: Found on the outer wall of the uterus, they often cause fewer symptoms.
While fibroids may not cause any symptoms, those that do can lead to problems like heavy menstrual bleeding, pelvic pain, and frequent urination. Submucosal fibroids, in particular, are most commonly associated with symptoms, and they often require surgical intervention for relief.