Introduction
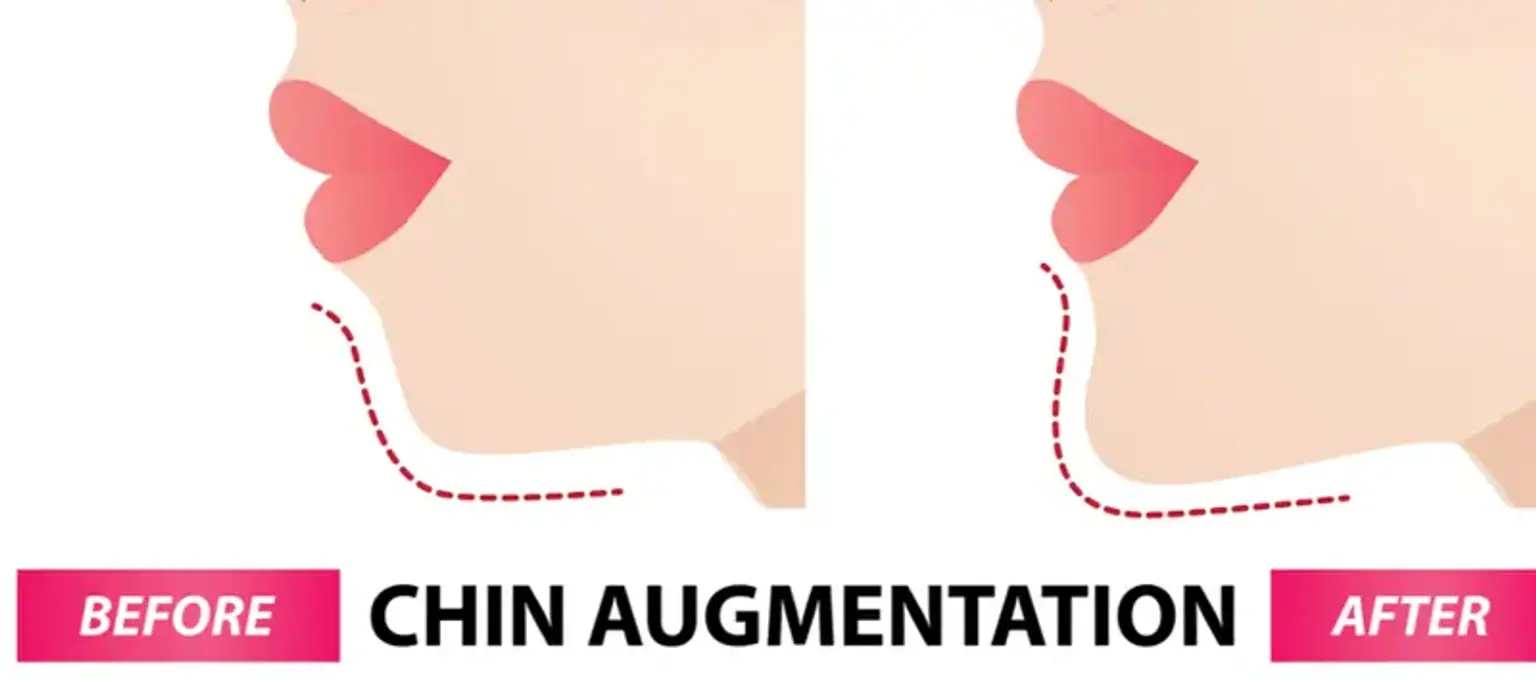
Chin augmentation surgery has become a popular solution for individuals seeking to enhance their facial profile and achieve a more balanced, harmonious look. Whether through chin implants or more advanced techniques like sliding genioplasty, this procedure helps improve the shape and projection of the chin, which in turn can have a significant impact on overall facial symmetry. For many, a defined chin can improve facial proportions, complementing other features such as the nose and jawline. As a highly customizable procedure, chin augmentation offers a range of options to meet individual aesthetic goals. This article explores the details of chin augmentation surgery, including the process, benefits, risks, recovery, and how it compares to non-surgical alternatives, helping patients make an informed decision for their cosmetic journey.
Understanding the Anatomy of the Chin
The chin plays a crucial role in overall facial aesthetics. Its size, shape, and position directly influence how the face looks, particularly in relation to the nose and eyes. A recessed chin, for instance, can make the nose appear more prominent, while a pronounced chin can help define the jawline. By repositioning the chin, chin augmentation surgery can improve facial symmetry and enhance the lower third of the face, making it more proportional to the rest of the features. For many patients, this results in a more youthful and attractive appearance, while also improving confidence.
Who is an Ideal Candidate for Chin Augmentation Surgery?
Ideal candidates for chin augmentation surgery are generally those with a chin that is underdeveloped or disproportionately small. This can be due to genetics, aging, or injury. To be considered a good candidate, a person should be in good overall health, have realistic expectations, and understand the potential risks involved. It is also important to have a stable mental health state, as cosmetic surgery can sometimes impact self-image. Chin augmentation is often combined with other facial procedures like rhinoplasty (nose job) to achieve overall facial harmony, particularly for those seeking more dramatic changes to their appearance.