Gastrocele
Overview
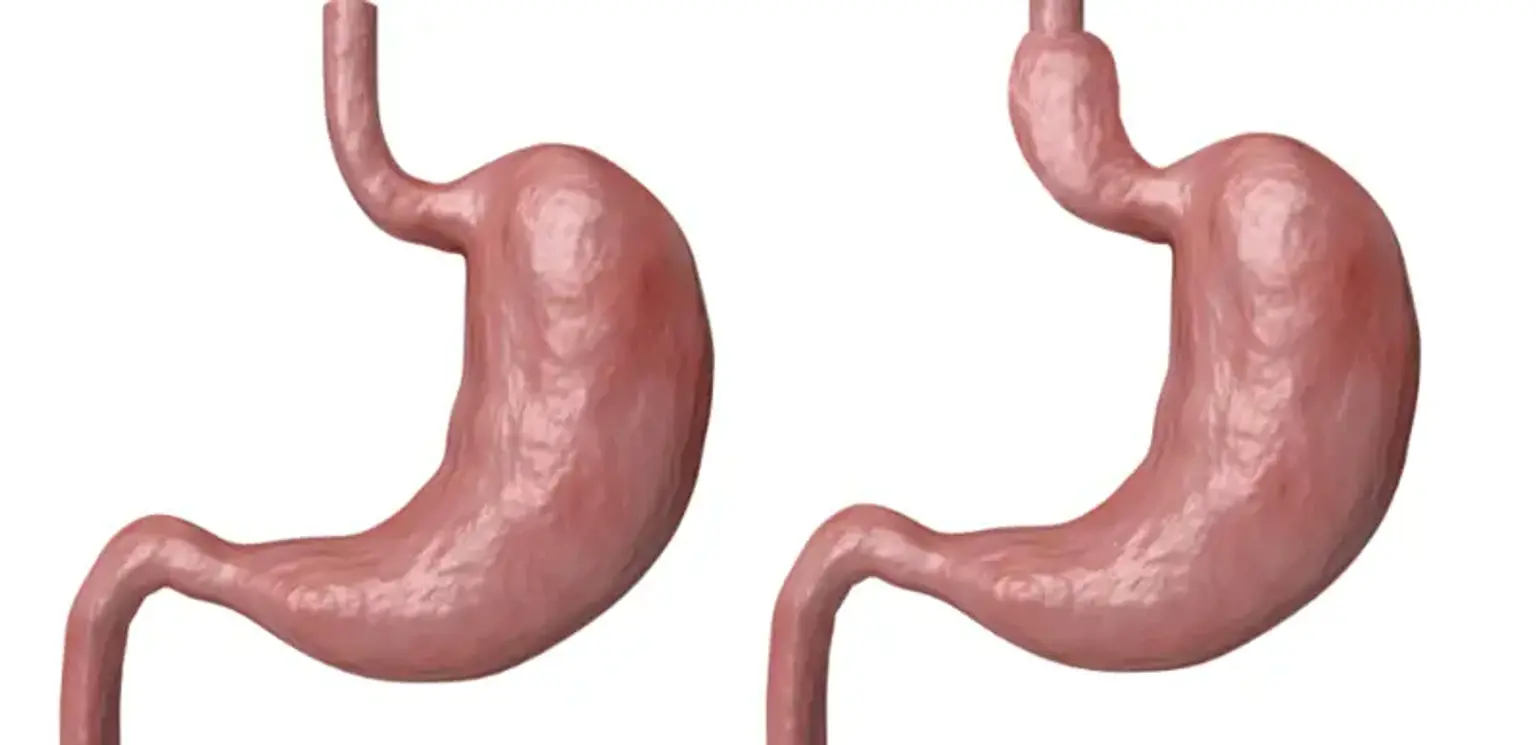
A hernia occurs when an organ protrudes through the muscle wall that surrounds it. A Gastrocele is a condition in which the upper part of your stomach protrudes into your chest, pushing through the small opening (or hiatus) in your diaphragm. Gastroceles are usually so small that they are not felt at all. However, if the hernia is larger, it may cause the opening in your diaphragm to expand as well. The entire stomach and other organs are in danger of sliding up into your chest at that point.