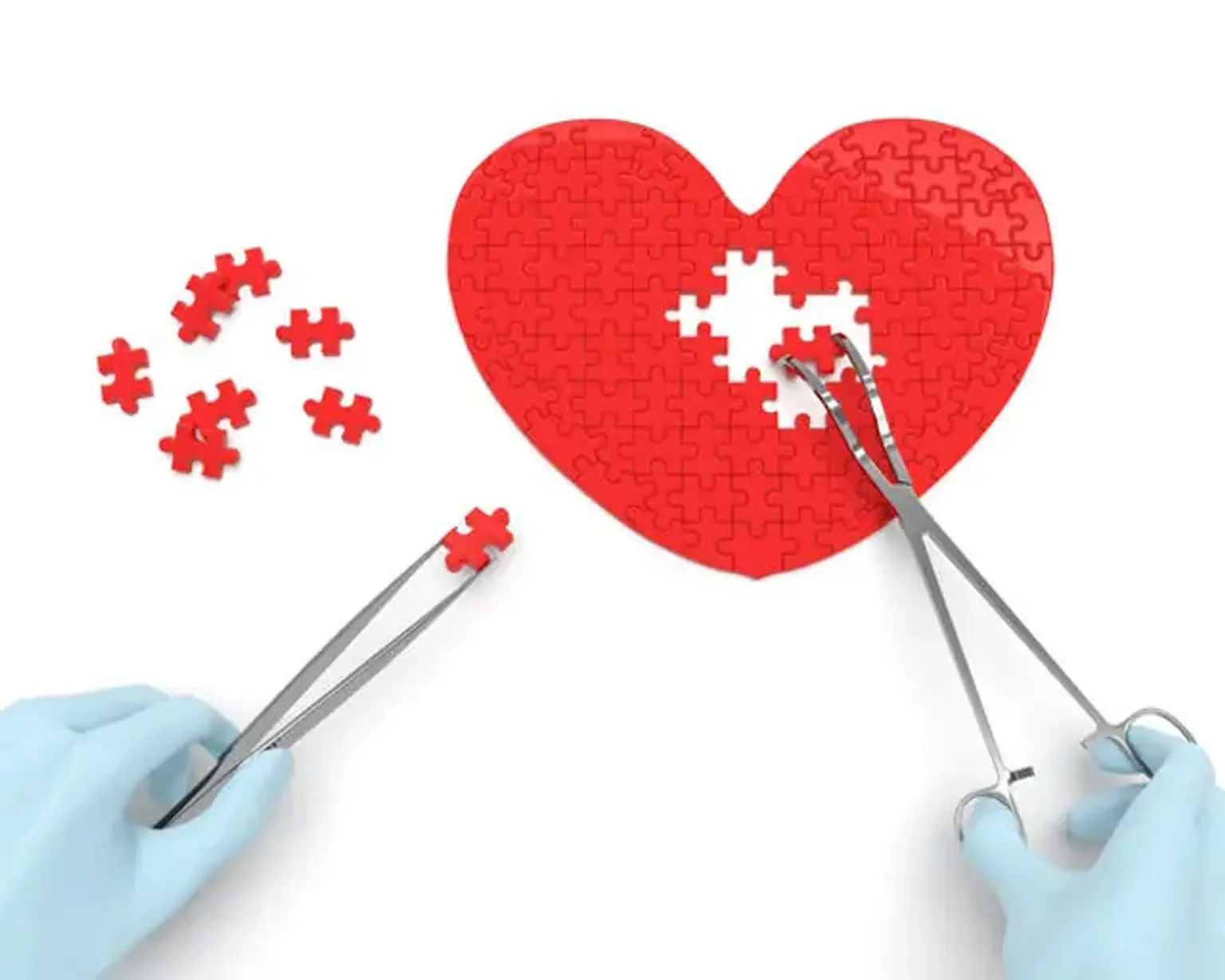
Heart Failure Surgery
Overview
Heart failure, also known as congestive heart failure, happens when the heart muscle is unable to pump blood as efficiently as it should. When this happens, blood frequently backs up and fluid can accumulate in the lungs.
Shortness of breath, extreme fatigue, and leg edema are frequent signs and symptoms of heart failure. Shortness of breath is frequently worse after activity or while lying down, and it might wake you up at night. A restricted capacity to exercise is another common symptom. Chest pain, especially angina, is not usually caused by heart failure.
The severity and etiology of the condition determine treatment. The majority of persons with heart failure do not require surgery and will be managed with medications. Heart surgery is only performed when doctors believe it can relieve a problem with the heart valves or the heart's blood supply, and only if the heart is strong enough. In most situations, surgery will not be able to treat heart failure.