Hepato-Pancreato-Biliary Surgery
What is the Hepato-Pancreato-Biliary Surgery?
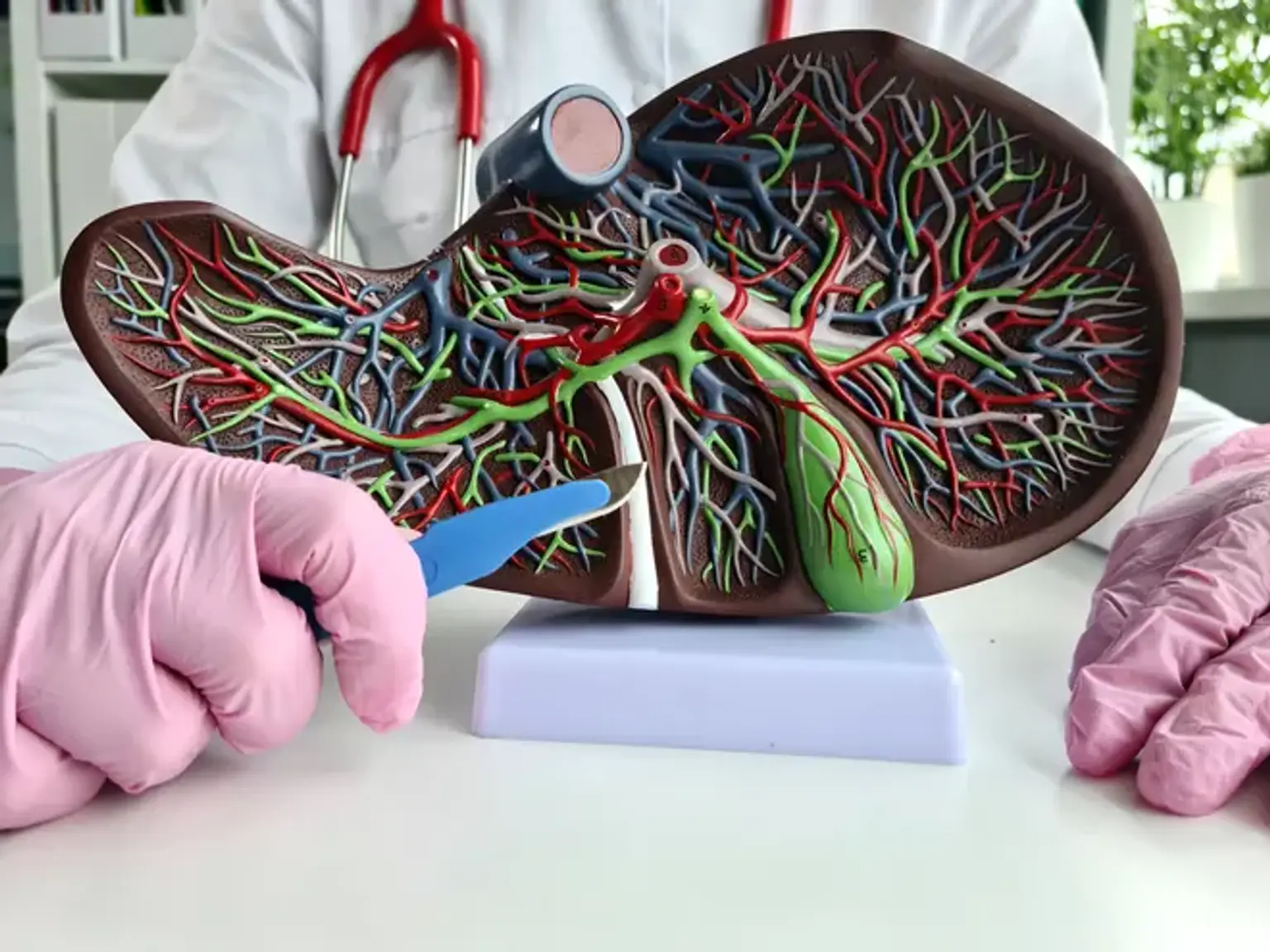
The liver, gallbladder, bile ducts, and pancreas make up the hepatobiliary system. This system is necessary for fat digestion and waste removal in the body.
The liver is a major organ on the right side of your stomach. It is divided into two sections: the right lobe and the left lobe.
The gallbladder is a tiny, pear-shaped organ located under your liver that your body utilizes to store bile. The gallbladder also contributes in bile formation and transportation. Bile is produced in the liver and released after you eat to aid in the digestion of fat and certain vitamins.