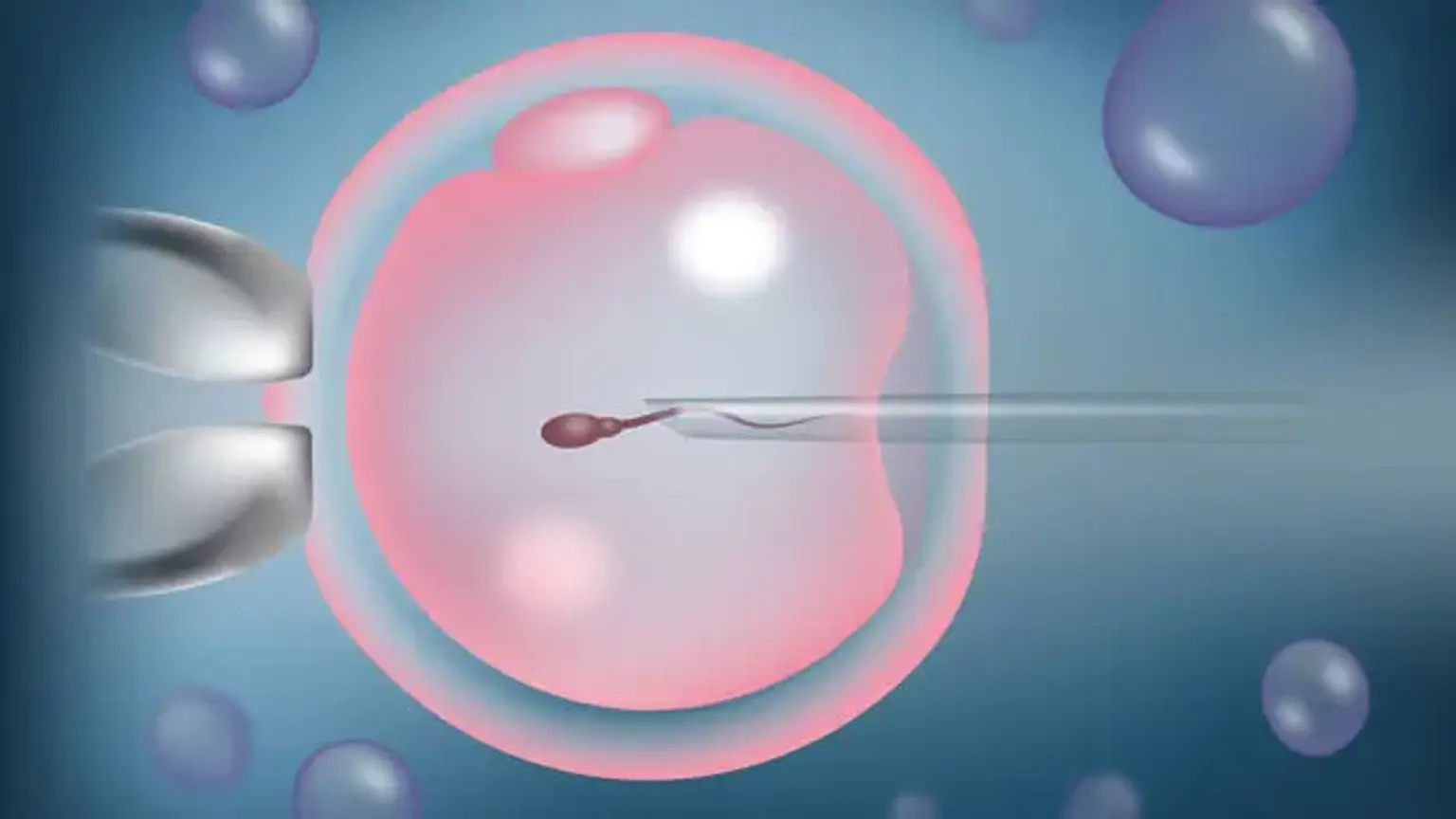
ICSI (Intracytoplasmic sperm injection)
Overview
Infertility is a complicated issue that may be caused by a number of circumstances, including male or female partners. Fortunately, in addition to intracytoplasmic sperm injection and in vitro fertilization, there are a variety of fertility therapies available to assist couples fulfill their desire of motherhood.
Intracytoplasmic sperm injection is indicated for couples who have been diagnosed with male reproductive difficulties such as low sperm count, low sperm morphology or motility, anti-sperm antibodies, or who have previously had a vasectomy or vasectomy reversal that was unsuccessful.