IgA nephropathy (Berger's disease)
What is Berger's disease?
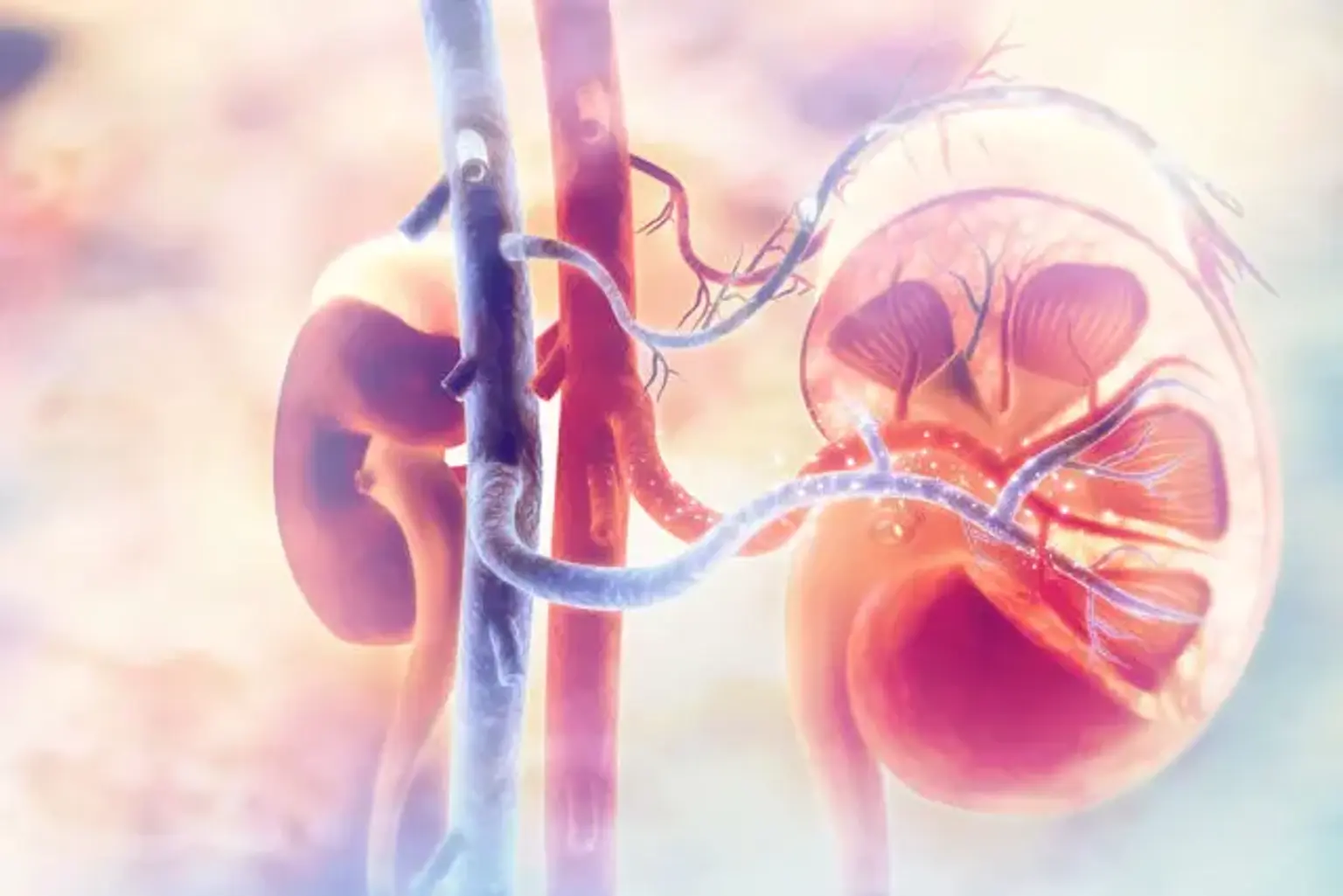
IgA nephropathy can also be referred to as Berger's disease. It’s a type of kidney condition that damages the small tiny filters of the kidneys. IgA nephropathy arises when the antibodies known as immunoglobulin A (IgA) accumulate in the kidneys. Immunoglobulin forms part of the normal areas of the body's immune system that facilitate infection and microorganisms fighting function. Patients with IgA nephropathy usually have a defense mechanism version of immunoglobulin A.