Inflammatory Diseases
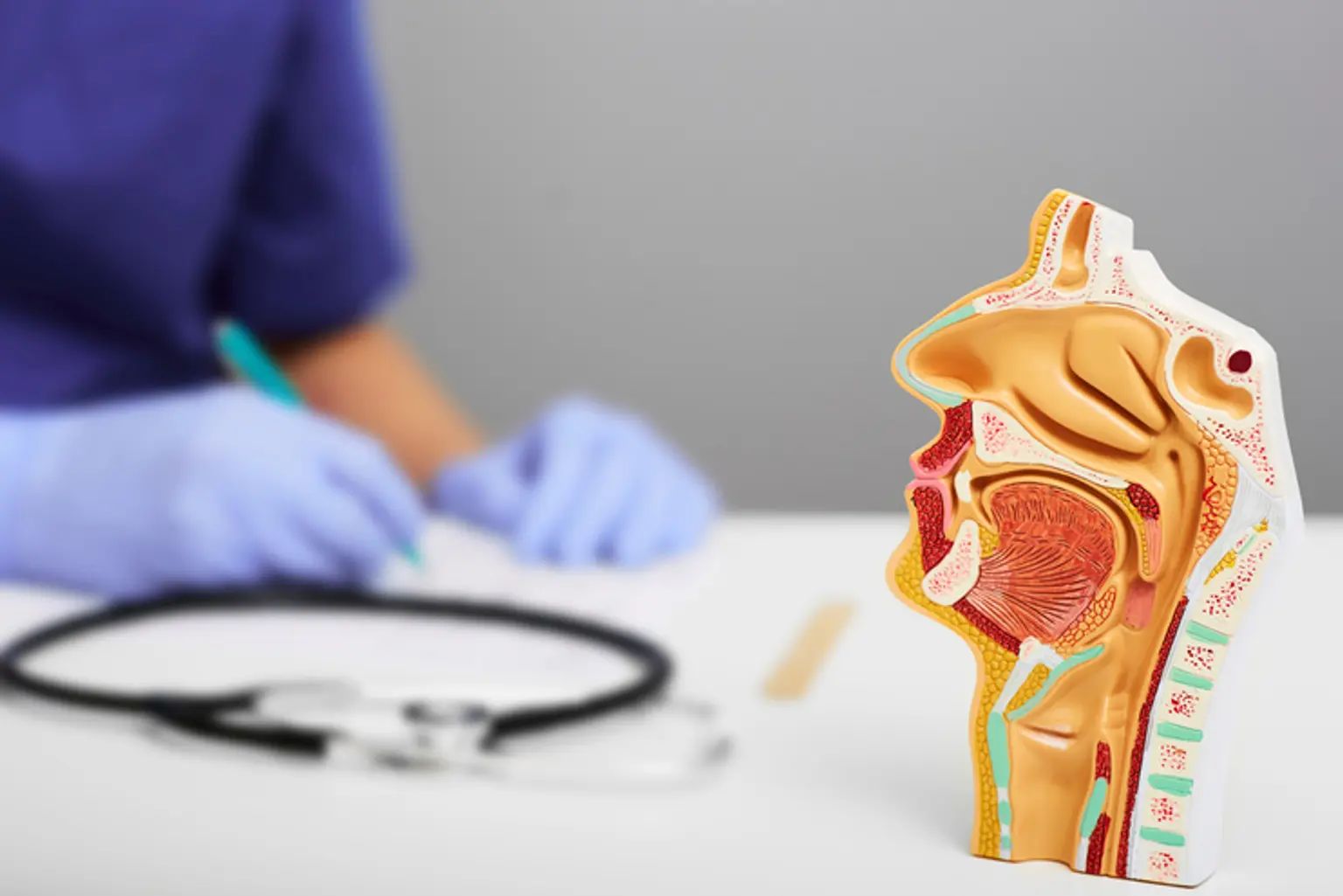
The sensory organs that are a part of the face and neck are the ear, nose, and throat. Some important head structures, such as the sinuses and Eustachian tubes, are common among them. Many ears, nose, and throat (ENT) issues can affect people, and clinicians sometimes group these illnesses. The ear, nose, and throat may be impacted by several conditions. While some ENT issues are simple, others can be trickier and involve different body systems. Many ENT problems can be treated by a general practitioner; however, certain patients may need to consult a specialist for a proper diagnosis and treatment plan.