Inflammatory heart diseases
Overview
Pericarditis, myocarditis, and endocarditis are all examples of inflammatory heart disease (IHD). Although males tend to be more afflicted than females, IHD can affect people of any age. While the sickness may be self-limiting and lead to complete recovery, afflicted individuals may acquire chronic disease, implying that identifying key triggers is crucial for successful therapy. Adding to the complication is the fact that IHD can be caused by a range of viral and non-infectious causes, as well as sequel events following main injuries.
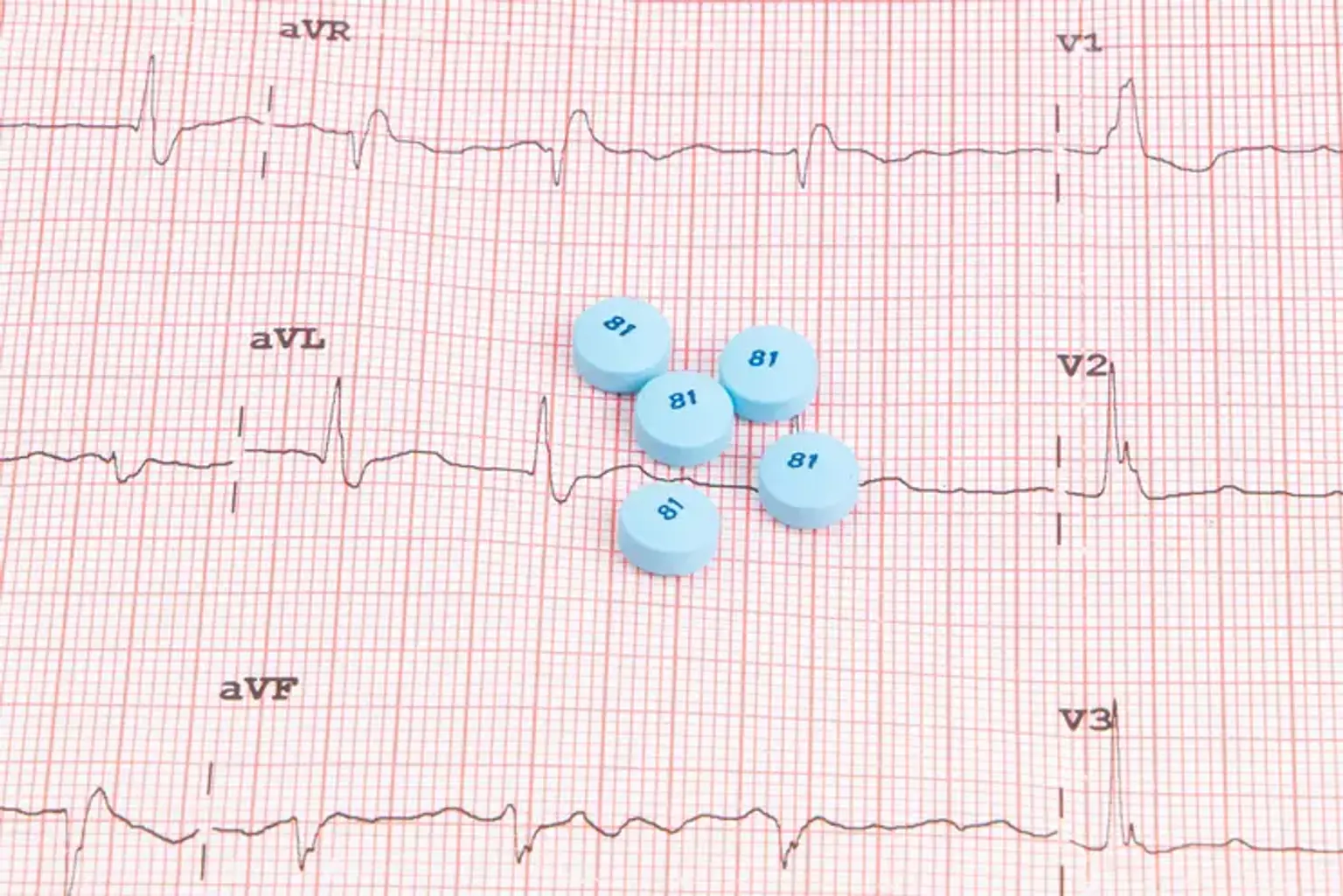
Myocarditis, or inflammation of the myocardium, can be caused by a variety of pathogens, including bacterial, rickettsial, mycotic, protozoan, and viral agents. The disease's clinical presentation is exceedingly diverse, ranging from nonspecific flu-like symptoms to arrhythmias, palpitations, disorientation, and syncope, as well as left ventricular failure.