Laparoscopic Ovarian Cystectomy
Overview
The majority of women will develop an ovarian cyst at some time in their life. Cysts typically generate little to no symptoms. If a cyst is causing pain or discomfort, surgical excision of the cysts may be the best therapeutic choice. Pelvic discomfort, especially during your period or sexual intercourse, is one of the signs of an ovarian cyst.
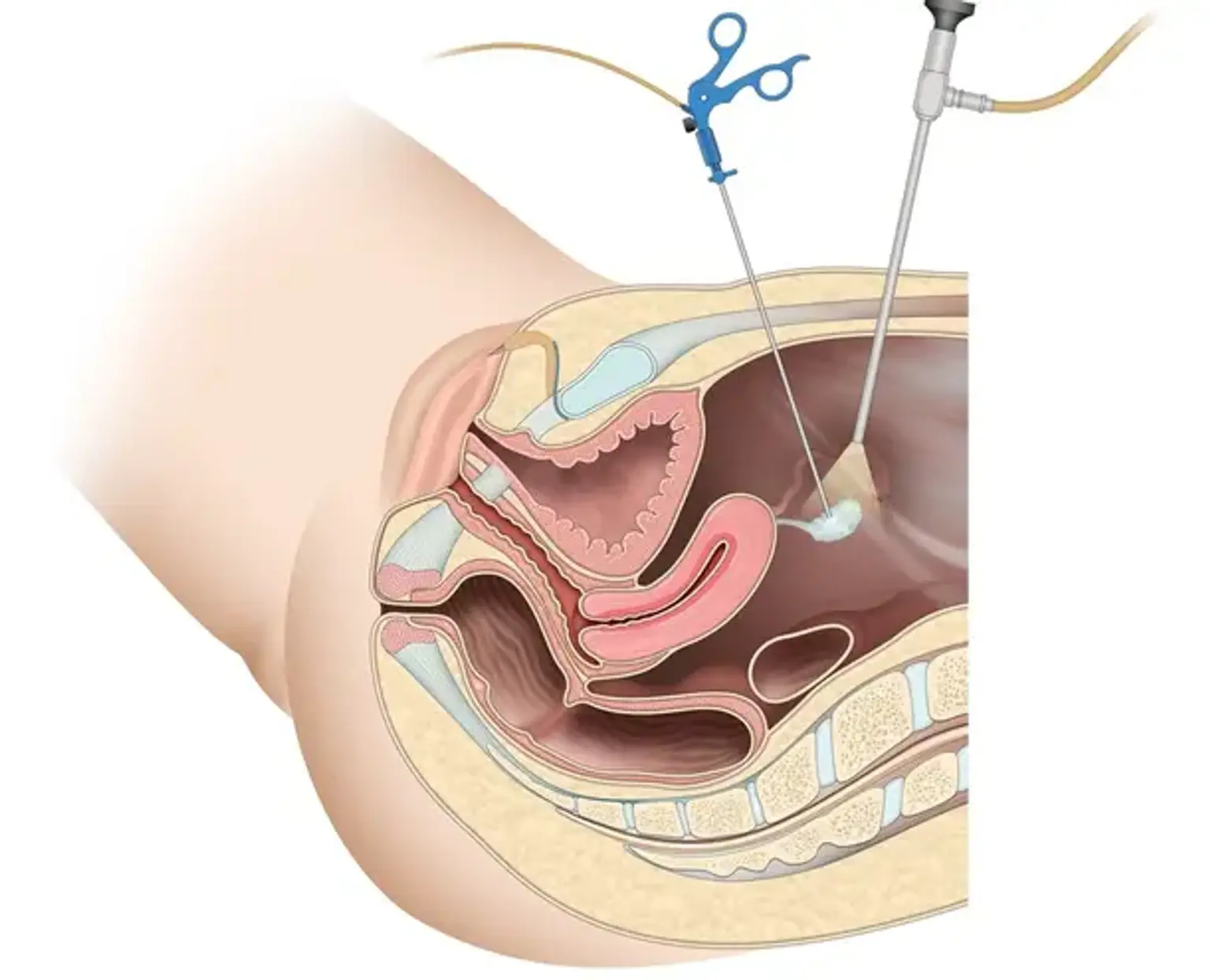
An ovarian cystectomy is a surgical procedure that removes a cyst from your ovary. Laparoscopic surgery is a type of minimally invasive surgery that requires only a few tiny incisions in your lower abdomen.