Laparoscopic Pyeloplasty
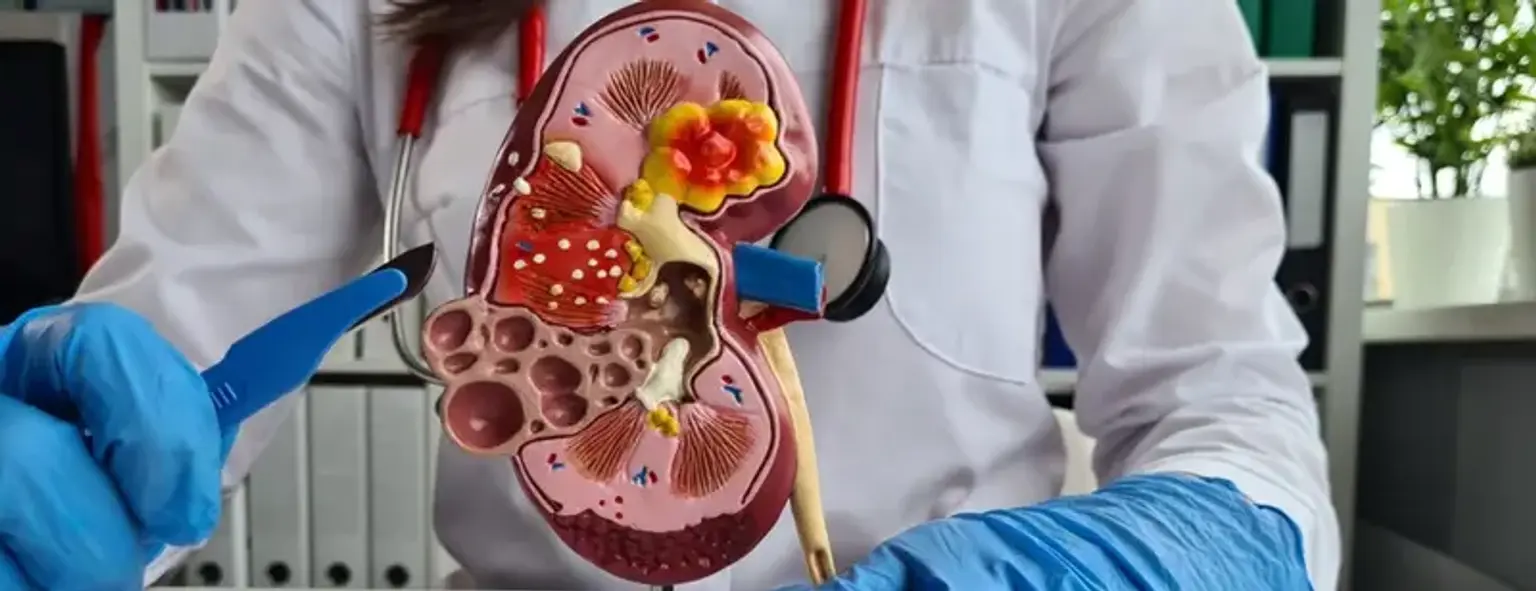
Reconstructive surgery can be carried out safely and effectively for patients with laparoscopic pyeloplasty. shrinkage or scarring where the ureter links the kidney with a minimally invasive treatment (the ureter is the tube that empties the kidney to the bladder). It is applied to fix ureter obstructions or narrowing that develop as the ureter exits the kidney. This anomaly, known as a hitch of the ureteropelvic junction (UPJ), causes a weak and sluggish urine flow from the kidneys. A UPJ obstruction may result in flank and abdominal pain, kidney dysfunction, infections, high blood pressure, and renal stones. Laparoscopic pyeloplasty has many advantages over open surgery, including much less postoperative pain, a shorter hospital stay, quicker return to work and normal activities, and cosmetic results that are just as good.