Introduction
Laparoscopic fallopian tube removal, also known as tubectomy, is a minimally invasive surgery used to treat various gynecological conditions that affect the fallopian tubes. This procedure involves the removal of one or both fallopian tubes through small incisions in the abdomen, with the assistance of a camera and specialized surgical tools. Compared to traditional open surgery, laparoscopic surgery offers significant advantages, such as smaller scars, quicker recovery, and reduced risk of complications.
This surgery is commonly performed for women who suffer from conditions like infertility, chronic pelvic pain, ectopic pregnancy, or pelvic inflammatory disease (PID). In many cases, laparoscopic fallopian tube removal is a necessary step toward improving a woman’s health and quality of life, while also potentially enhancing fertility outcomes in certain cases.
What is Laparoscopy and How Does it Work?
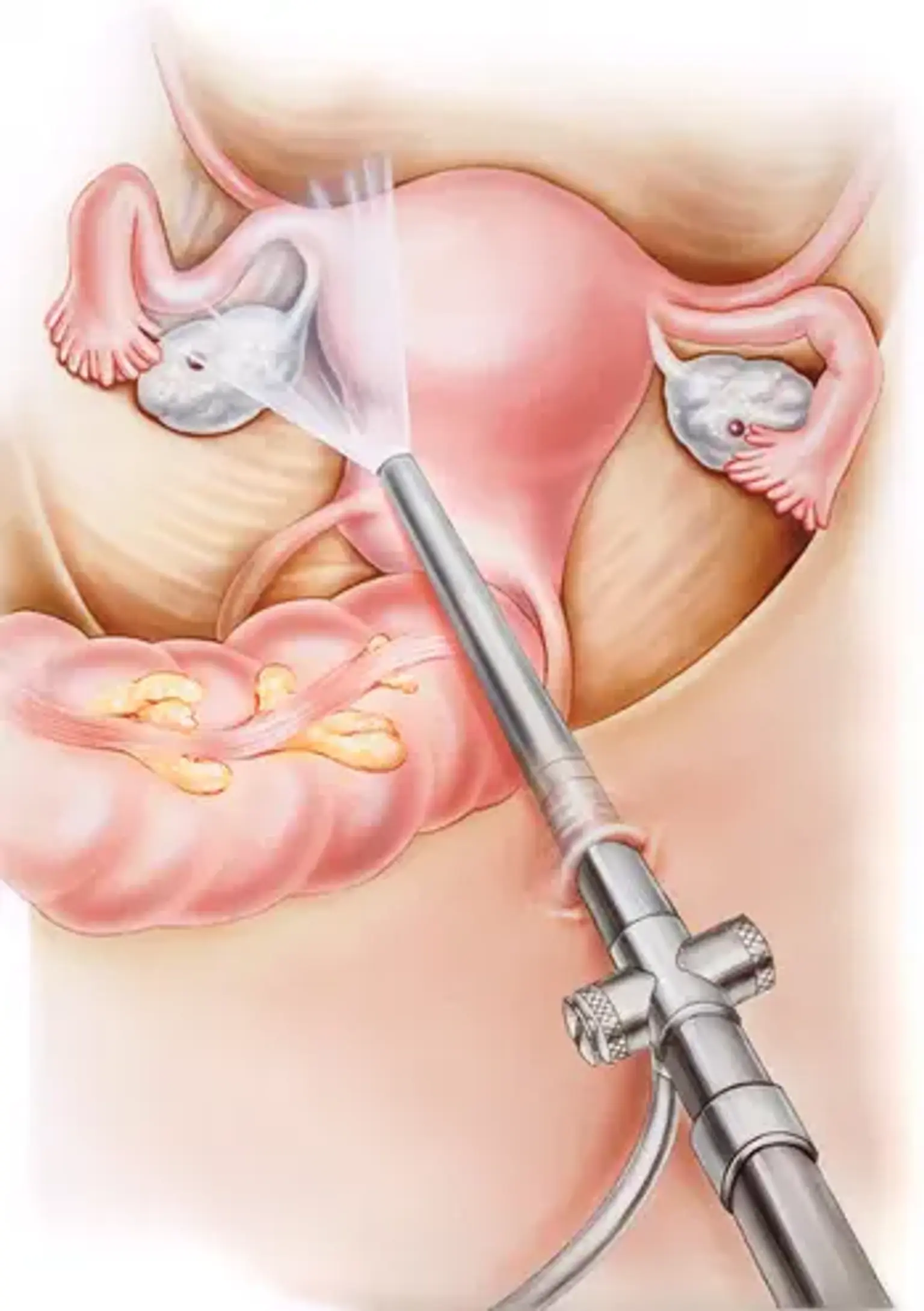
Laparoscopy is a type of minimally invasive surgery that allows surgeons to perform complex procedures with just a few small incisions. A laparoscope, a thin tube with a light and camera at the end, is inserted into the body, giving the surgeon a clear view of the pelvic organs on a monitor. Using this technology, surgeons can precisely remove the fallopian tubes without the need for large incisions, reducing trauma to the body and speeding up recovery.
This technique is widely used for gynecological surgeries because it offers several benefits over traditional open surgery. The smaller incisions result in less bleeding, reduced scarring, and lower risks of infection. Recovery time is also significantly shorter, meaning patients can usually return to normal activities much sooner.
Indications for Fallopian Tube Removal
There are several medical conditions that may necessitate the removal of the fallopian tubes, either to treat disease or prevent further complications. Common reasons for fallopian tube removal include: