Introduction
Overview of Cervical Health and Dysplasia
Cervical health is a crucial aspect of a woman’s overall well-being, and regular screenings can help detect any abnormalities before they lead to more serious health issues. One of the most important tools in detecting cervical problems is the Pap smear, which screens for abnormal cells in the cervix. When abnormal cells are found, it can be an indication of cervical dysplasia, a condition where cells in the cervix begin to grow abnormally. If left untreated, cervical dysplasia can develop into cervical cancer.
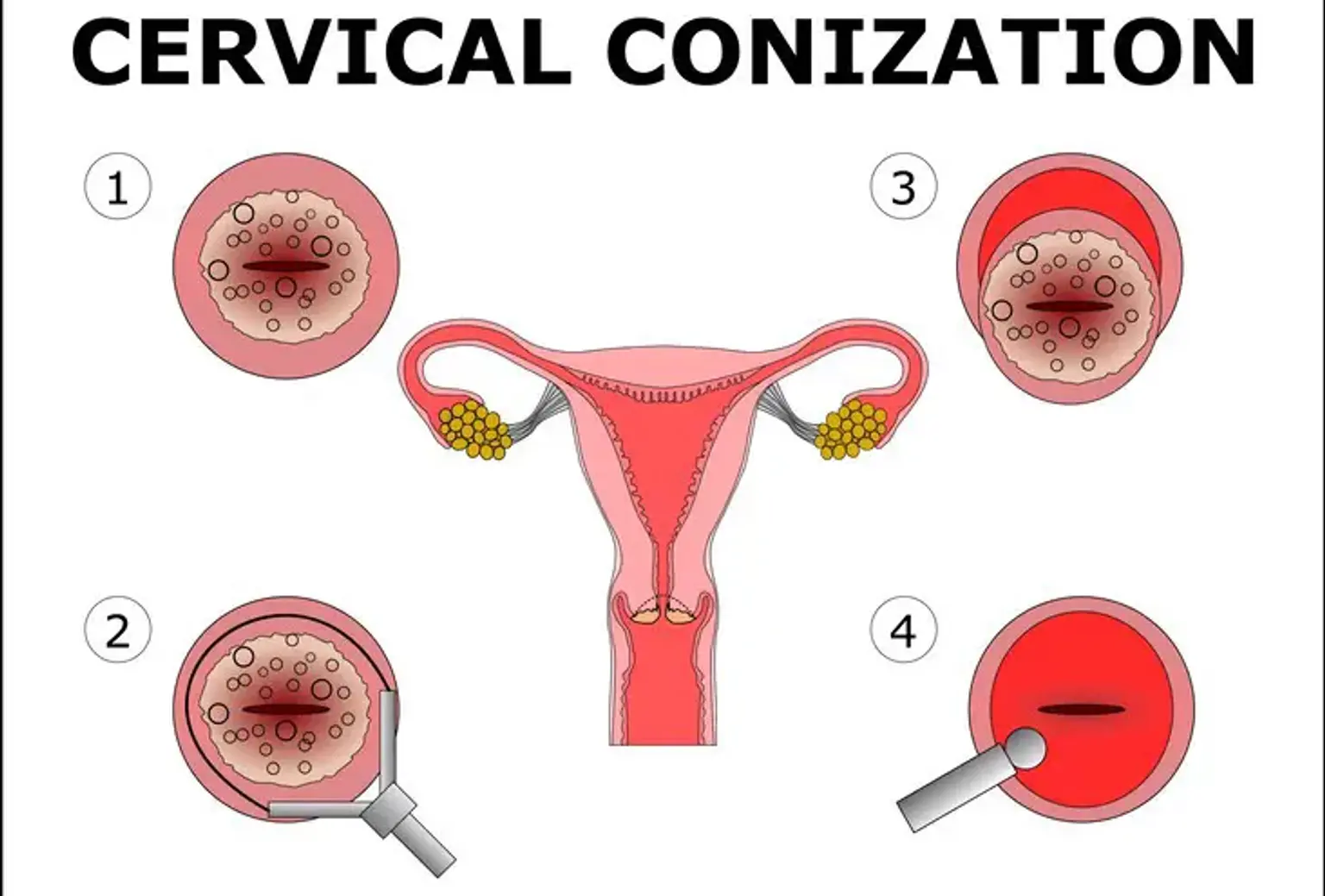
Early detection and intervention are key to preventing the progression of cervical abnormalities. Cervical conization, a medical procedure where a cone-shaped portion of abnormal tissue is removed from the cervix, plays a significant role in treating these abnormalities. Among the different methods for cervical conization, laser cervical conization is becoming increasingly popular due to its precision, effectiveness, and relatively quick recovery time.
What is Laser Cervical Conization?
Laser Cervical Conization is a minimally invasive procedure that uses a concentrated beam of laser light to remove abnormal tissue from the cervix. It is typically recommended for women with moderate to severe cervical dysplasia or precancerous changes detected during routine screenings like a Pap smear or colposcopy. The laser focuses on the abnormal cells, vaporizing or coagulating them, and leaving healthy tissue intact.
Laser conization is often preferred over other methods such as cold knife conization or loop electrosurgical excision procedure (LEEP) because of its precision. The laser can selectively remove the abnormal tissue with minimal damage to surrounding healthy tissue, which reduces the risk of scarring. This precision also minimizes the risk of bleeding, making the procedure safer and more effective for many women.
The procedure is an outpatient treatment, meaning patients can typically go home the same day, and it is performed under local anesthesia, making it less invasive compared to traditional surgical methods.