Lens Implantation
Overview
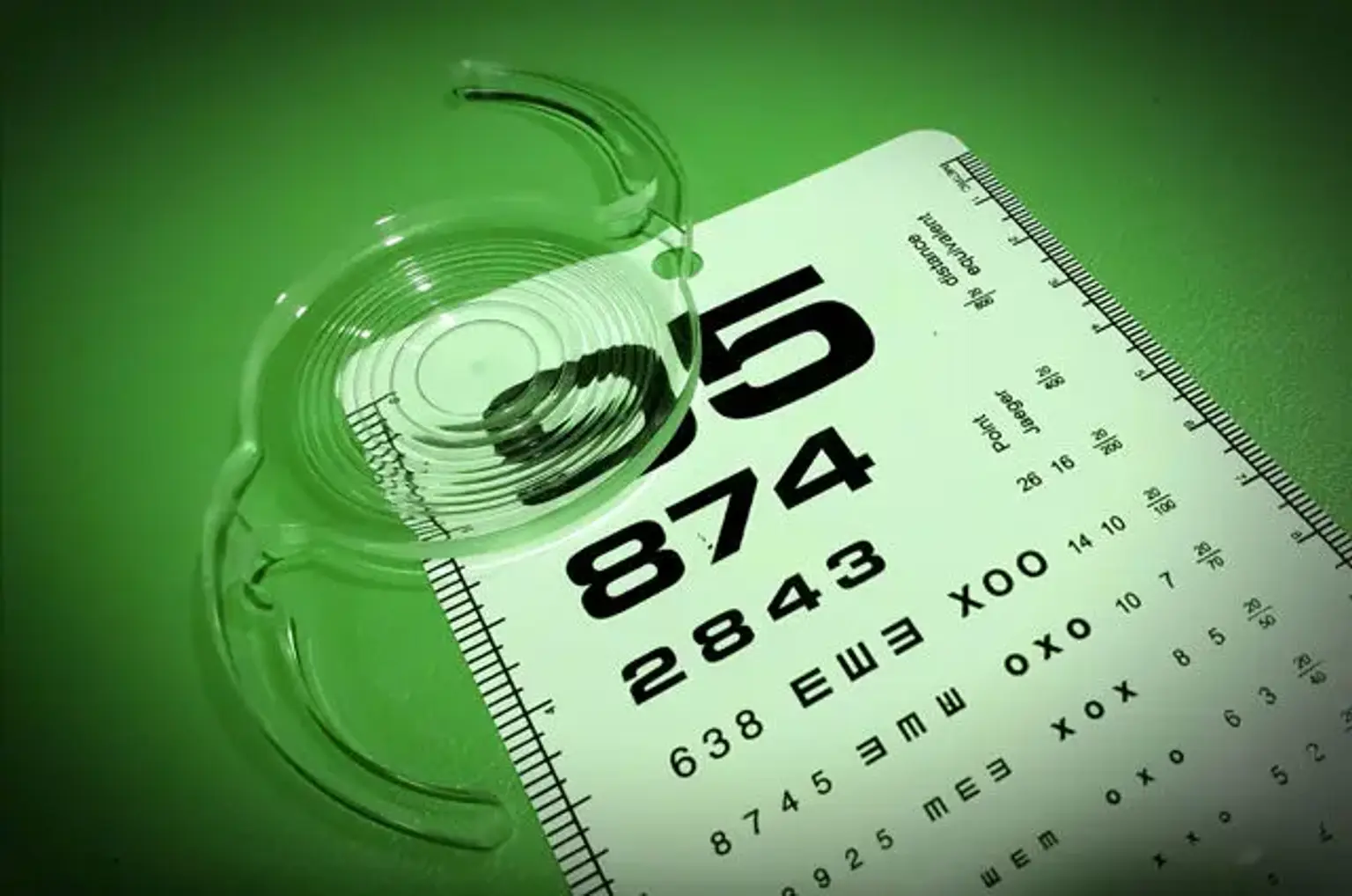
An intraocular lens (IOL) is a lens that is implanted in the eye to treat cataracts or myopia. If the natural lens is retained, the IOL is referred to as phakic; otherwise, it is referred to as a pseudophakic, or false lens. After the eye's hazy natural lens (colloquially known as a "cataract") has been removed, such a lens is commonly implanted during cataract surgery. The pseudophakic IOL performs the same function as the natural crystalline lens in terms of light focusing. The phakic type of IOL is used in refractive surgery to modify the optical power of the eye as a therapy for myopia. It is put over the existing natural lens (nearsightedness).
IOLs are typically made up of a tiny plastic lens with plastic side struts called haptics that keep the lens in place inside the eye's capsular bag. IOLs were previously made of an inflexible material (PMMA), however this has been mainly replaced by the use of flexible materials such as silicone.
The majority of IOLs used today are fixed monofocal lenses designed for distance vision. Other types of intraocular lenses are available, such as multifocal intraocular lenses, which give multiple-focused vision at distant and reading distances, and adaptive intraocular lenses, which provide limited visual accommodation. Multifocal IOLs can also be Trifocal IOLs or have an extended depth of focus (EDOF) lens.