Liver Fibrosis
Liver fibrosis refers to scarring of the liver, one of the largest organs in the body. It is responsible for digestion, energy storage, formation of blood-clotting components, and removal of waste and bacteria, among other things. The liver can also repair injury or damage by regenerating or re-growing itself.
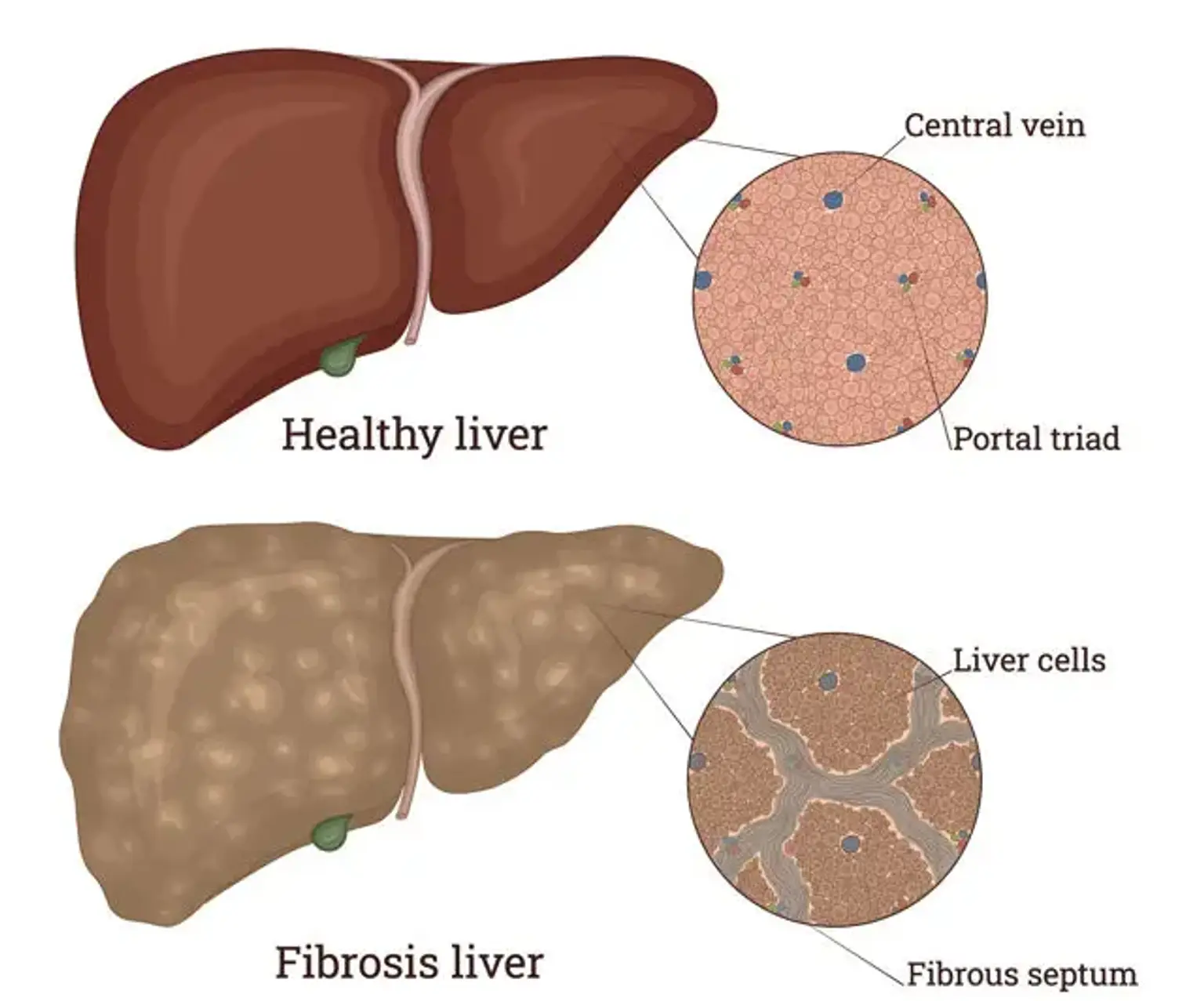
Liver fibrosis develops when scar tissue accumulates in the organ as a result of repeated or long-term damage or inflammation. Compared to healthy liver cells, Scar tissue cells are unable to repair themselves or operate in any other way. Fibrosis can lower the overall function of the liver and impair its ability to regrow as a result of this.
Fibrosis scar tissue can as well obstruct or restrict blood flow within the liver. This could starve and finally destroy the healthy cells, resulting in additional scar tissue.