Minimally invasive thoracic procedures (without opening the chest)
Overview
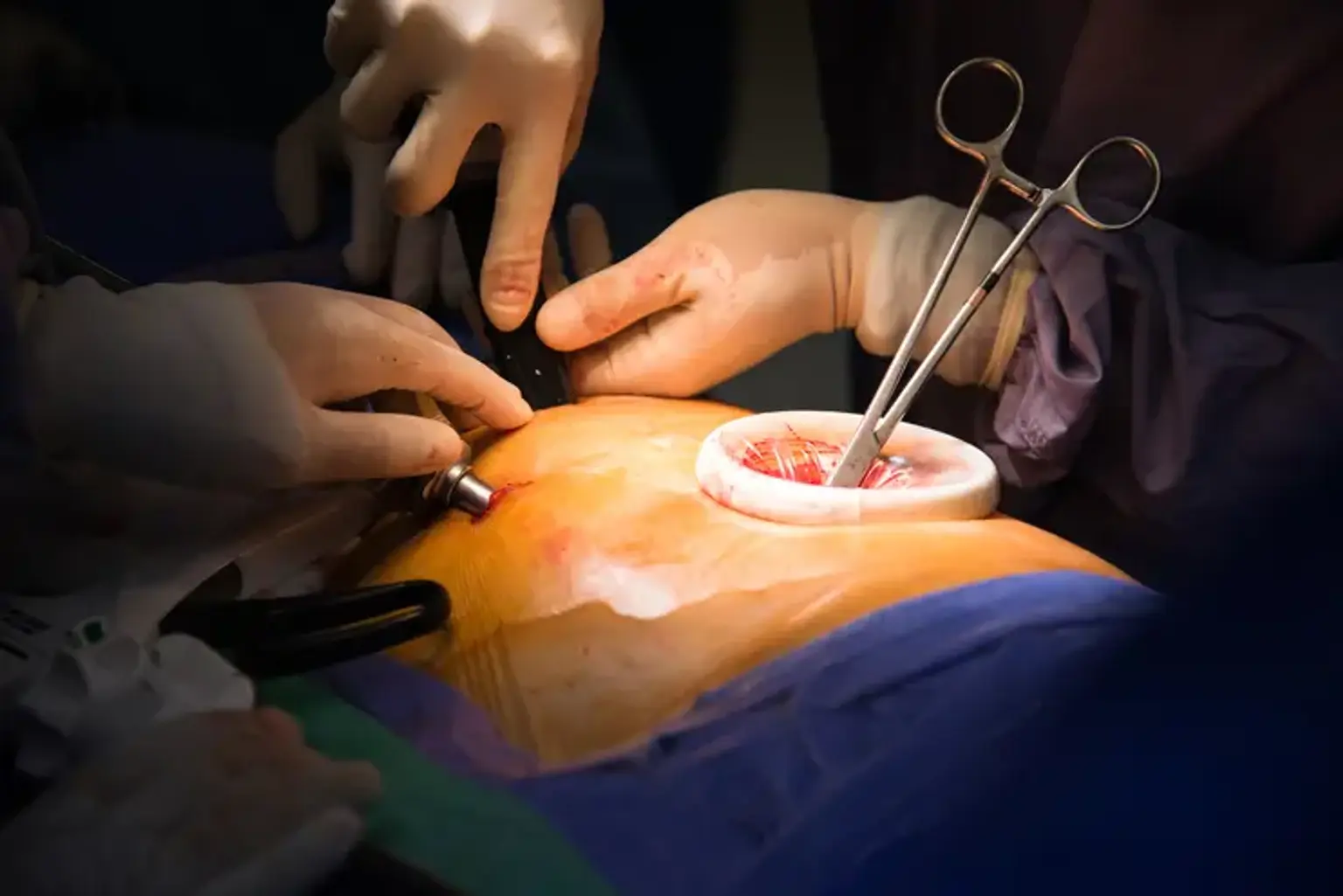
Thoracic surgery has changed throughout the years. Accessing the intrathoracic organs through the bony ribcage has proven problematic for thoracic surgeons. Large incisions across the chest, such as posterolateral thoracotomies with rib spreading, were the conventional way to accessing the lungs in the past. These procedures involve significant trauma to the patient and have high rates of death and morbidity.
However, as technology and surgical techniques have advanced, thoracic surgery has developed to reduce patient stress while still adhering to oncological and surgical principles. Modern technology, along with a wide range of old and new surgical procedures, provides the thoracic surgeon with a strong weapon.