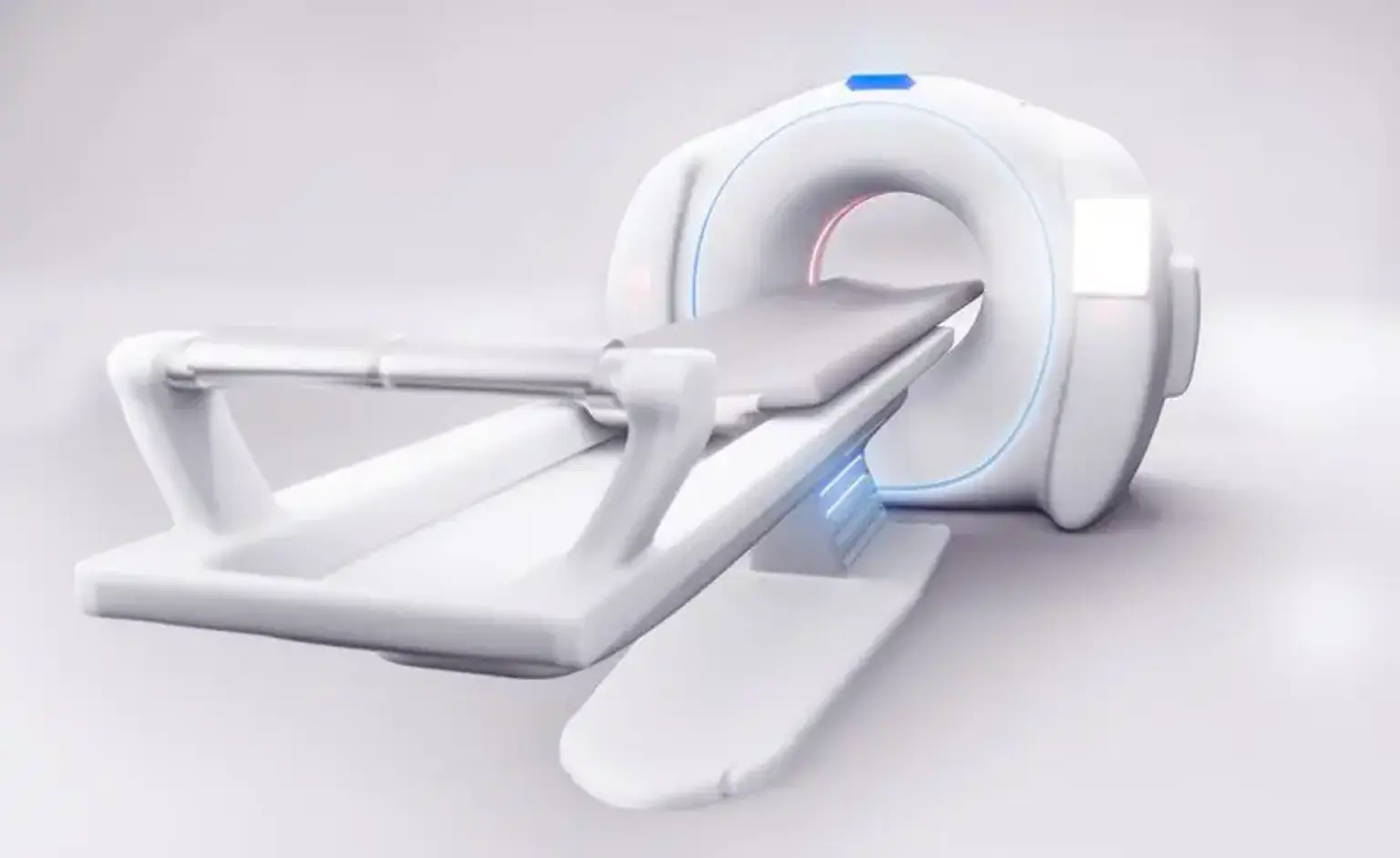
Multi-detector computed tomography (MDCT)
Overview
The invention of multidetector computed tomography (MDCT) is regarded as a significant advancement in CT imaging, with direct implications in the imaging of many systems, most notably the cardiovascular system. The benefits of MDCT include a significant improvement in image acquisition speed, increased patient coverage, and excellent spatial resolution.