Myeloproliferative disorders
Overview
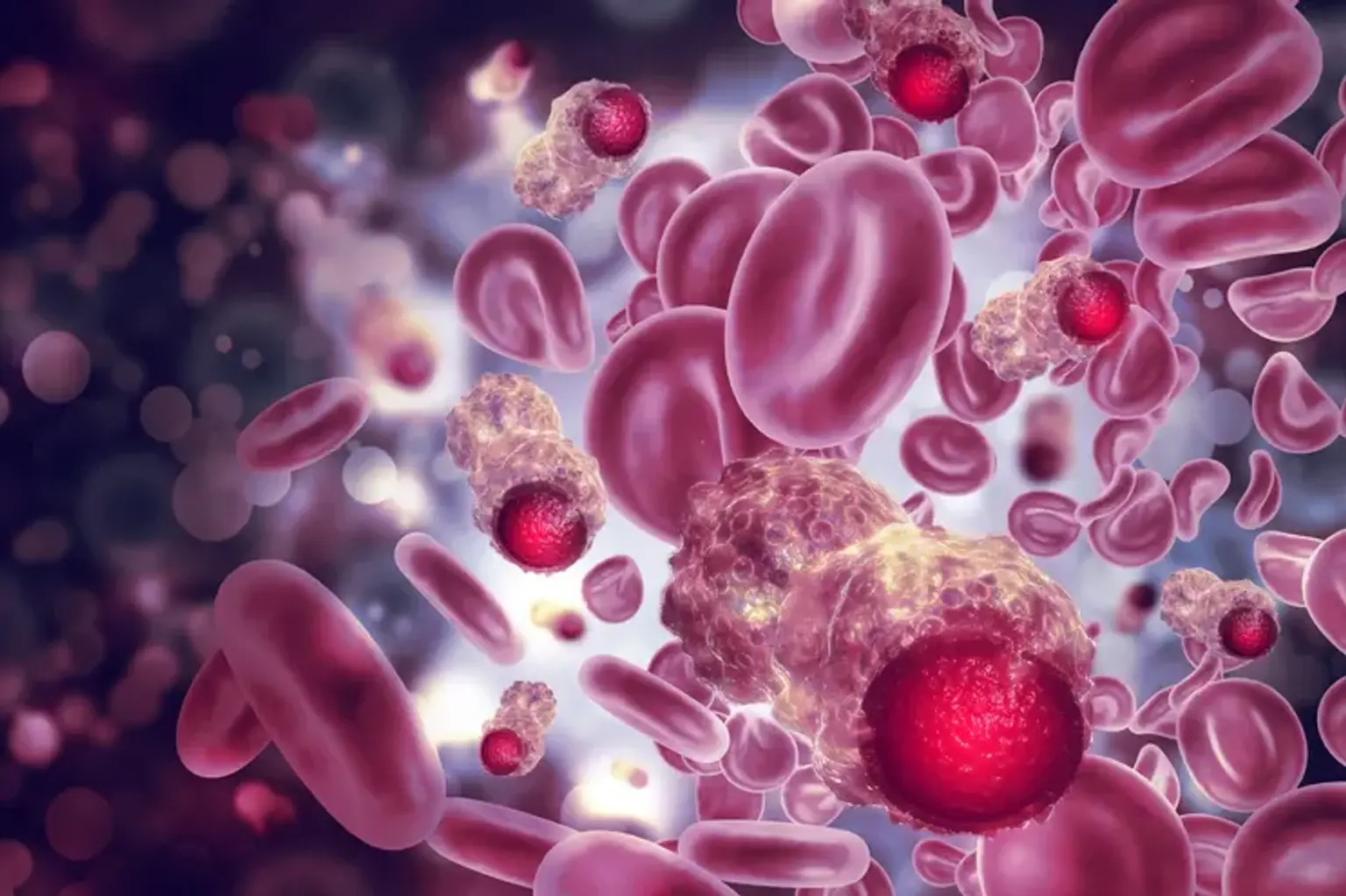
Myeloproliferative diseases are severe situations in which an abnormally large number of blood cells are generated. This can interfere with regular blood processes. Overactive signaling in blood-producing cells causes myeloproliferative diseases.