Introduction
Nasal polyps are noncancerous growths that form inside the nasal passages or sinuses, often as a result of chronic inflammation. These growths can block airflow and make it harder to breathe through your nose, leading to symptoms like nasal congestion, difficulty smelling, and sinus pressure. Though they may be small initially, untreated nasal polyps can grow and cause persistent discomfort.
Treatment for nasal polyps is essential to relieve symptoms, improve breathing, and prevent the condition from worsening. Options range from medications like nasal sprays and corticosteroids to surgical procedures for larger or recurrent polyps. Understanding your treatment options can help you manage the condition effectively and restore your quality of life.
What Are Nasal Polyps?
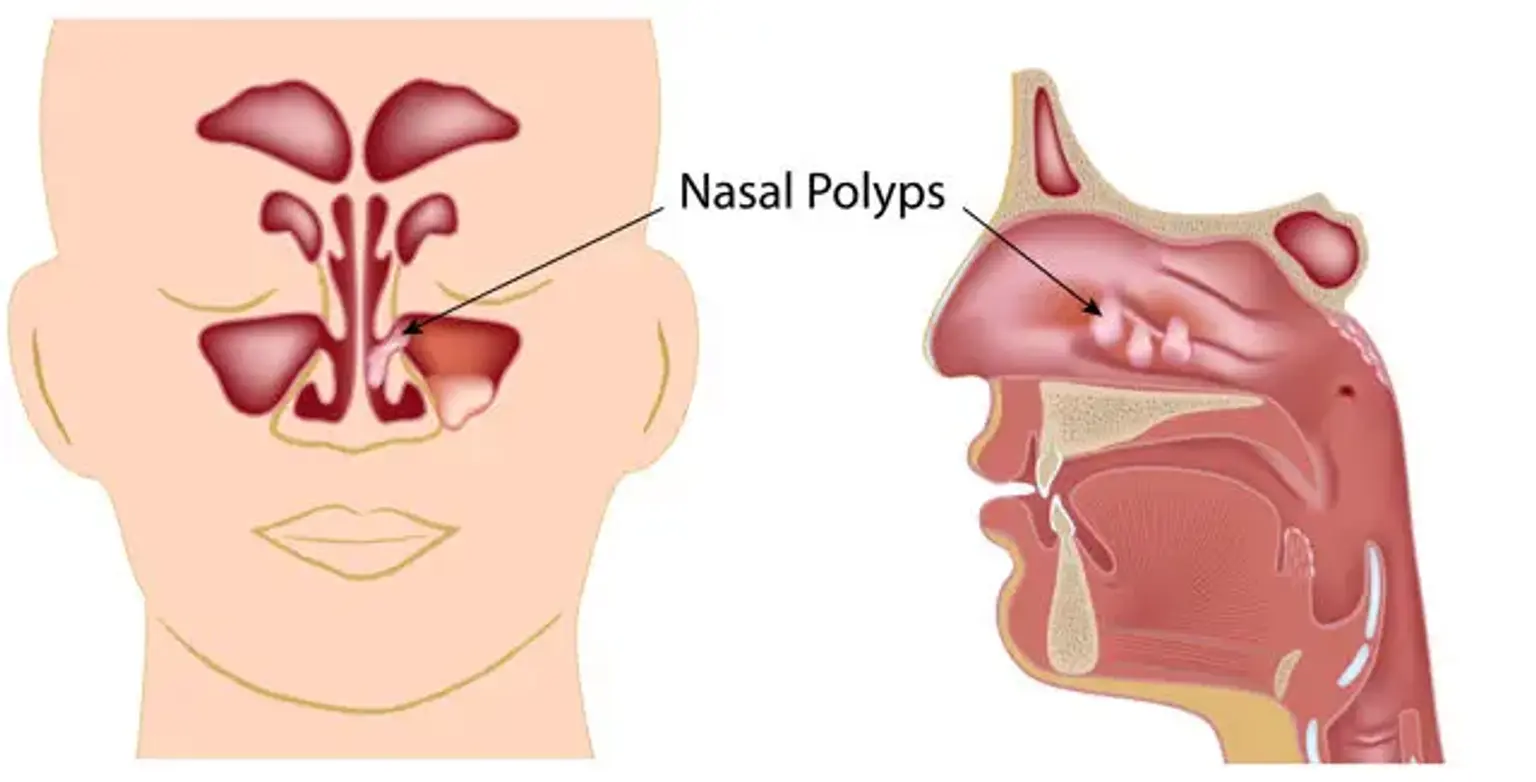
Nasal polyps are soft, painless growths that develop from the lining of your nasal passages or sinuses. They are typically associated with long-term inflammation, often due to conditions like chronic sinusitis or allergic rhinitis. Polyps can vary in size from small, seed-like structures to larger, more obstructive masses that block airflow.
The exact cause of nasal polyps is not fully understood, but they are believed to develop when the mucous membranes inside the nose and sinuses become inflamed over time. Inflammation causes the tissue to swell, eventually forming polyps. While anyone can develop nasal polyps, they are more common in people with asthma, allergies, or other chronic respiratory conditions.
Symptoms of Nasal Polyps
The most common symptoms of nasal polyps include: