Osteoarthritis
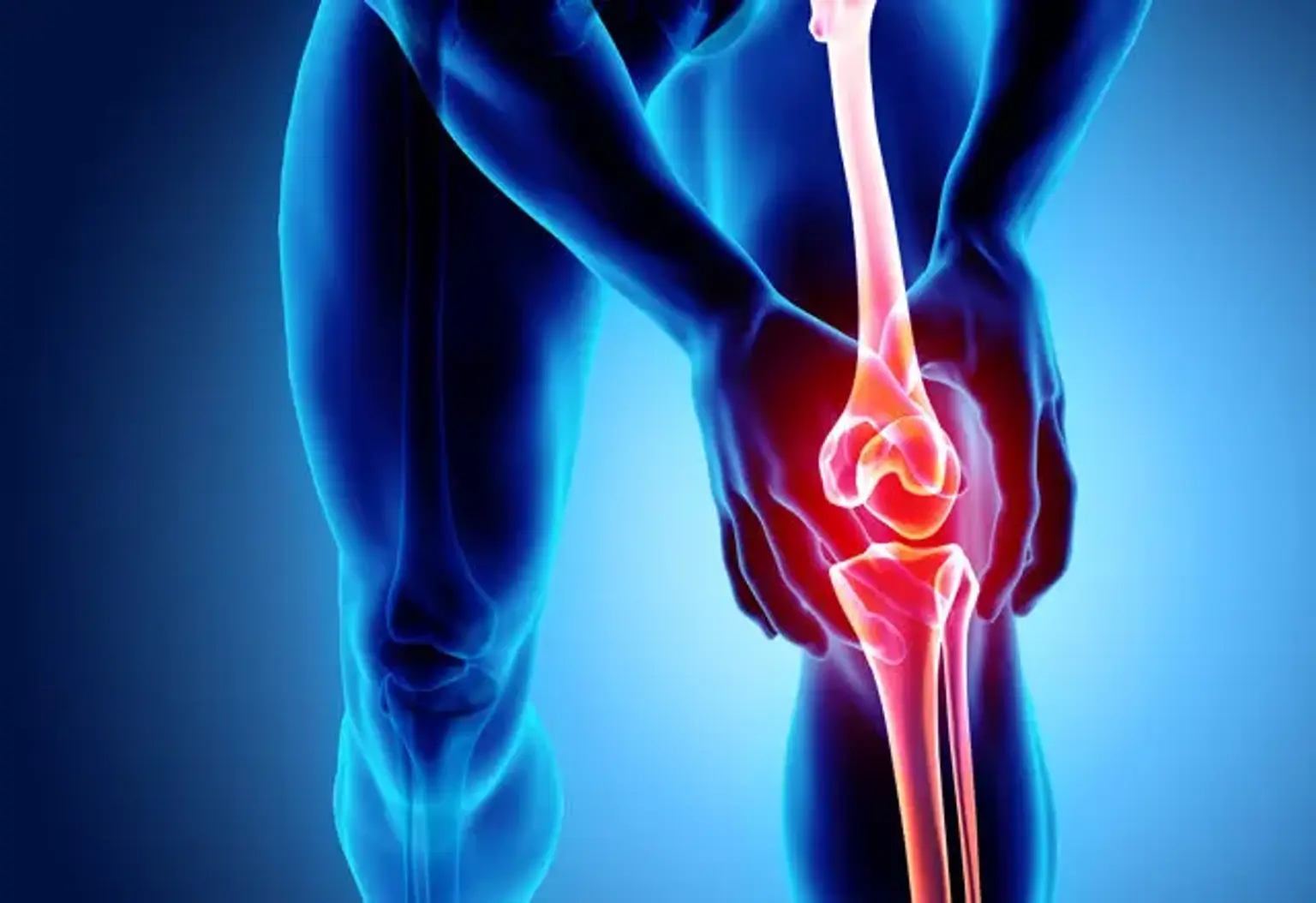
Osteoarthritis (OA) is one of the most prevalent types of arthritis that affects millions of people around the world. If the protective cartilage cushioning the tips of the bones wears down with time, it causes osteoarthritis. While osteoarthritis can affect any joint, it is most common in the hands, spine, knees, and hips.
As people grow older, the chances of developing osteoarthritis increase. Changes in osteoarthritis normally take several years to manifest, but there are exceptions. The damage and inflammation of the joint result in bony alterations, tendons and ligament deterioration, and cartilage degradation. This eventually causes joint pain, swelling, and even deformity.